Make the material too soft, and it can easily become damaged or degraded in the body. Make it too hard, and the prosthetic device is more likely to damage surrounding tissue.
Now researchers working in Switzerland and the U.S. have developed a spinal implant they hope will integrate into the central nervous system and function long term. Results of their study were published online in the journal Science on Jan. 9.
The new device, which approximates the shape and elasticity of human tissue, has enabled movement in rats paralyzed by spinal cord injury.
Chris Covington, DO, chief, section of inpatient rehabilitation, Spectrum Health Medical Group, said he was cautiously optimistic about the study results.
“We’ve seen positive short-term results before, but over time these devices all run into issues of immune rejection through damage to surrounding tissue,” he said. “An implant of this type that could function long-term without rejection by the body would be a significant development.”
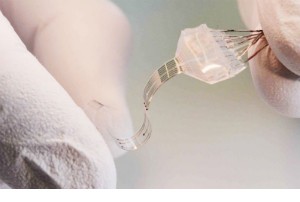
The key is in the material used to make their device, researchers say. It is soft and flexible, yet strong, like the body’s surrounding tissue. They call their implant “electronic dura mater,” (or e-dura) after the protective membrane of the brain and spinal cord. It can deliver both electrical and chemical stimulation while remaining fully elastic.
E-dura integrates a 120-millimeter-thick transparent layer of silicone with stretchable gold interconnects, soft electrodes coated with a platinum-silicone composite and a compliant microfluidic channel. The interconnects and electrodes transmit electrical impulses and transfer electrophysiological signals. The microfluidic channel allows drugs to be administered at the site of the implant.
This integrated design enables multiple applications to the surrounding tissue, resulting in the restoration of movement to paralyzed rats over weeks of implementation without damage to the spinal cord.
“The effective biomechanical, chemical and electrical integration between implants and neural tissues is critical to obtaining long-term results,” Dr. Covington said.
The study promises additional features for the device, which depend on further technological developments. These include the integration of tissue-matched implants with higher electrode density and implantable pumps for drug delivery.
Embedded electronics could allow researchers to control movement in real time and holds promise for the treatment of a wide range of diseases, including epilepsy, Parkinson’s disease and pain management.
 /a>
/a>
 /a>
/a>
 /a>
/a>