At just 5 weeks old, William “Alexander” Neal developed a small, nickel-sized bump on his jaw.
His parents, Hannah and William Neal, had no idea where it came from.
“We had to take him to the emergency room,” William said. “He was getting so grumpy and the bump was even pushing his tongue to the other side of his mouth.”
William and Hannah drove Alexander an hour to the emergency department at Spectrum Health Helen DeVos Children’s Hospital, where he underwent imaging and analysis.
The bump was a tumor.
Doctors at the children’s hospital sent Alexander to the pediatric intensive care unit for observation overnight and scheduled a biopsy on the tumor for the next day.
“The nurse on the floor was such a blessing to have on that day,” Hannah said. “It was the worst night of my life and she helped me get through it.”
As the mass grew, it had begun to push on Alexander’s airway. Doctors placed him on a ventilator.
His doctors believed it could be infantile fibrosarcoma, but they needed to await confirmation from the biopsy before they could begin treatment.
Right medication, right time
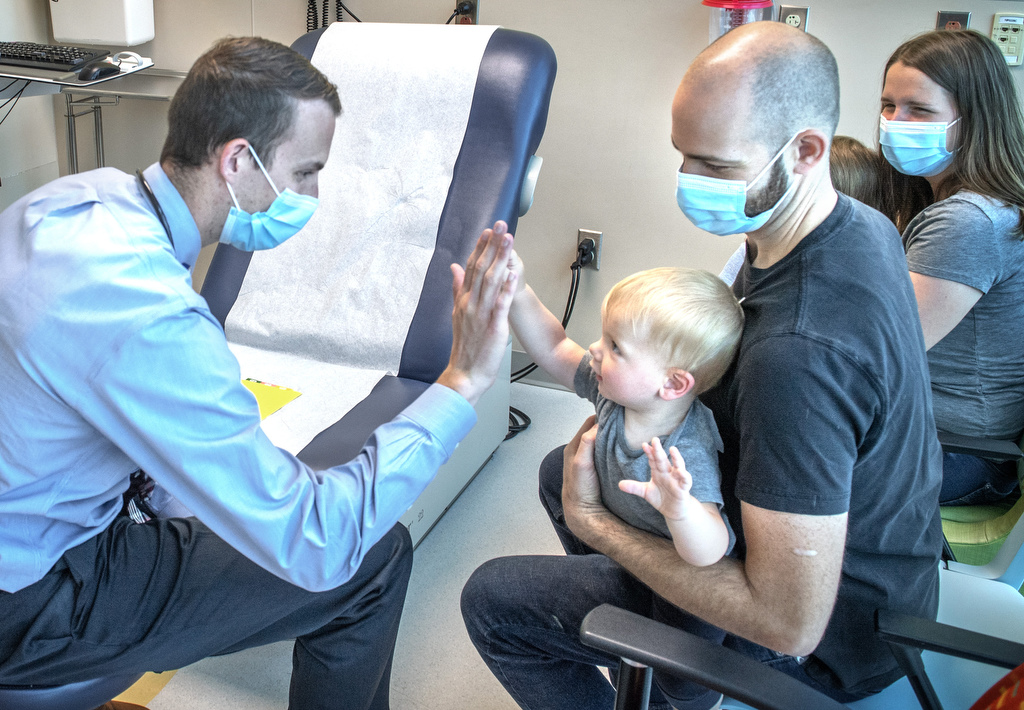
David Hoogstra, MD, principal investigator at the Haworth Innovative Therapeutics Clinic at Helen DeVos Children’s Hospital, and Deanna Mitchell, MD, pediatric oncologist at Helen DeVos Children’s Hospital, knew the exact drug that would help Alexander.
Precision medicine, which identifies the specific genetic mutation involved and the appropriate treatment, helped pave the way.
Julie Steinbrecher, a clinical research nurse at Helen DeVos Children’s Hospital, worked to get the ball rolling to gain quick access to the drug, larotrectinib, which is highly effective at treating this kind of cancer.
Another benefit: In addition to being extremely effective against Alexander’s infantile fibrosarcoma, larotrectinib has far fewer side effects than the traditional chemotherapy medicines used to treat this cancer prior to the discovery of this drug.
It was a race against time, Dr. Hoogstra said.
“We had confirmation of infantile fibrosarcoma within 48 hours,” Dr. Hoogstra said. “The hero of this story is Nurse Julie, as she got the ball rolling on this medication early on and asked for it to be sent ASAP for such a critical situation.”
The same day that doctors confirmed the cancer diagnosis, the drug arrived at the hospital.
Alexander would begin treatment immediately.
“It was one of those miraculous things,” William said.
“It almost felt like we were in a movie,” Dr. Hoogstra said. “Everything came together in such perfect timing.”
‘It’s completely gone’
Incredibly, just 24 to 48 hours after starting treatment, the tumor on Alexander’s cheek had shrunk.
“It had shrunk so quickly, we decided to do a repeat CT scan,” Dr. Hoogstra said.
The care team had considered inserting a tracheostomy tube in Alexander’s neck to help him breath on his own, anticipating it could be weeks to months before the tumor would shrink enough for him to fully breath on his own.
But his sudden improvement changed all that.
“It had shrunk so dramatically we were able to remove the breathing tube,” Dr. Hoogstra said.
So just days after beginning treatment, Alexander could breathe on his own.
“Tumors, like sarcomas, just don’t shrink this fast with standard treatment,” he said. “Before precision medicine, patients would need a port and would get chemotherapy, which usually comes with side effects. And the time to see a response like this could take months.”
Just months later, radiologists could find no trace of Alexander’s tumor.
“It’s completely gone after about four months on treatment,” Dr. Hoogstra said. “He’s in remission with no evidence of the tumor.”
“We’ve been so blessed,” Hannah said. “We were able to go home six days after he started the medication, and it’s now shrunk so small you can’t even see it.”
William, an ICU nurse who has also worked as a paramedic, described the experience with Alexander as extremely humbling.
“Seeing this happen to my own family … to my son … and not being able to do anything was really hard,” William said. “It was very difficult for me to not have answers or know myself. But we were so thankful for the amazing support and care at the hospital.”
Alexander now continues to take medication, which Dr. Hoogstra believes he’ll need to continue taking for a year.
“We had the right medication for the right kind of cancer at the right time,” William said. “It was just amazing.”
‘Overlapping blessings’
Alexander is back home with his family.
He’s growing well. He’s crawling. He’s meeting all his developmental milestones.
“From birth until Alexander was off the breathing support, he was increasingly grumpy,” Hannah said. “But he is just such a happy and smiley baby ever since his tumor has shrunk.”
A small scar on his face is the only visible sign of his battle with cancer.
“Dr. Hoogstra knew about the medicine and was familiar with this kind of cancer,” Hannah said. “We were so blessed to be at Helen DeVos Children’s Hospital and to have access to these doctors who knew about rare cancers.”
“The number of overlapping blessings is just amazing,” William added.
Having a child diagnosed with cancer can be one of the hardest things for a family to experience, Dr. Hoogstra said, and he is continually inspired by their resilience and courage.
And, amid it all, precision medicine is playing a leading role in shaping positive outcomes.
It’s an exciting time for precision medicine, said James Fahner, MD, division chief for pediatric hematology and oncology at the Ethie Haworth Children’s Cancer Center at Helen DeVos Children’s Hospital.
“This is truly the new era of cancer therapy that we have all patiently awaited, and fervently prayed for,” Dr. Fahner said. “It is literally precision medicine, personalized medicine, at its very best.”
Care teams are using the most innovative molecular diagnostic techniques to help pinpoint the exact mutation responsible for fueling the growth of the cancer cells, Dr. Fahner said.
Armed with this knowledge, they’re able to target that mutation with exquisite precision.
“Sparing these vulnerable children the risks and side effects of aggressive surgery, chemotherapy and radiation,” Dr. Fahner added. “Their story is indeed a miracle of modern medical science.”
Dr. Hoogstra echoed his enthusiasm for the future of personalized medicine.
“It’s a really exciting time to be a pediatric oncologist,” Dr. Hoogstra said. “With precision oncology, we are using cutting-edge molecular testing to understand these specific genetic changes leading to each patient’s unique cancer.
“And our hope is to personalize individual treatment to provide the best care for each patient.”



























 /a>
/a>
 /a>
/a>
 /a>
/a>
Praising God for the miracle! Alexander looks so big now! What a precious “young man!”