For most women, periods last three to five days.
That’s how it had always been for Chris Groenheide—until she hit age 50.
“I had a period that began on May 21, 2016, and it lasted until Oct. 18, 2016,” she said.
At first, Chris, now 53, didn’t pay much attention to the bleeding. She’d hit the age when many women experience menopause, so maybe it had something to do with that.
Or maybe not.
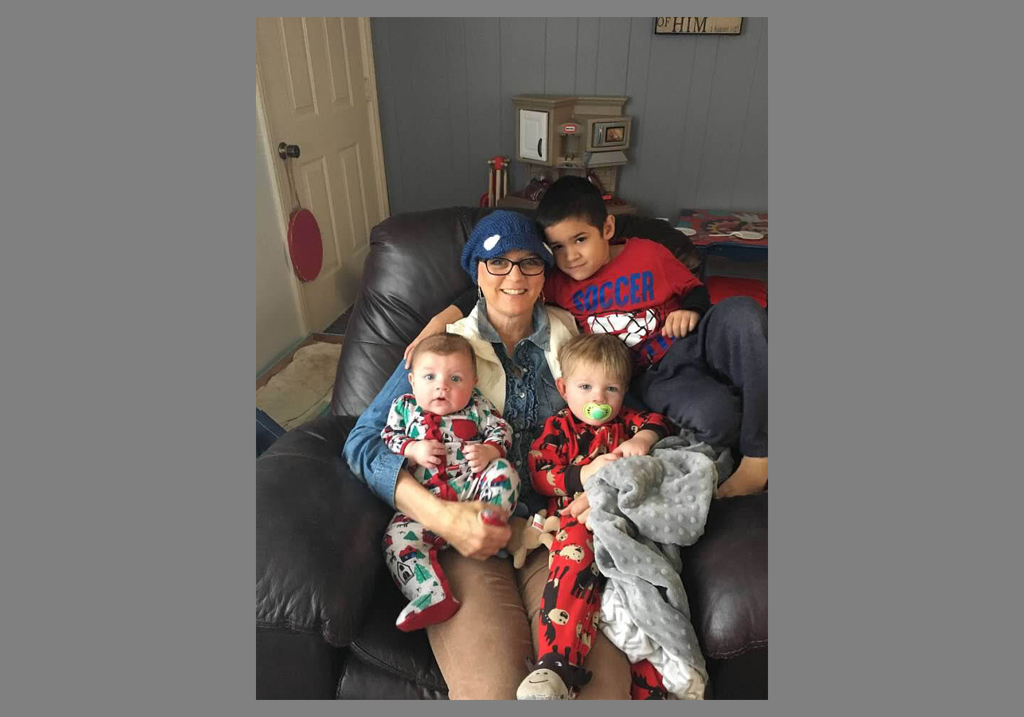
A former paraprofessional at the school district in Byron Center, Michigan, Chris had retired to take care of her grandsons. Her role as a grandmother brought her great joy, which meant her focus had remained largely on the boys—not on her own health.
But then the bleeding increased. And she began to notice blood clots.
In the thick of things
In July 2016, Chris went to see her gynecologist. An ultrasound revealed an enlarged uterus with a thickened lining.
“My gynecologist prescribed meds to slow the bleeding,” Chris said. “She didn’t suspect cancer because I had none of the risk factors. She thought maybe my progesterone—the hormone involved in my menstrual cycle—was off and the meds would adjust that.”
Chris wasn’t the typical age for uterine cancer and she wasn’t overweight. She also lacked the type of family history that would have put her in a high-risk group.
Still, something seemed off.
“I went camping with the family, but when everyone went swimming I stayed on shore,” Chris said. “I was still bleeding too much. I wasn’t in pain but I was feeling tired. Probably anemic by then.”
In September 2016, Chris had a second ultrasound.
Her gynecologist referred her to Leigh Seamon, DO, MPH, a specialist in gynecological oncology at Spectrum Health. Dr. Seamon had immediate concerns about the thickened lining of Chris’ uterus.
“It was 38 millimeters thick,” Dr. Seamon said. “A normal uterine lining is around 5 millimeters thick or less for postmenopausal patients.”
When Chris got into the stirrups for a pelvic exam, Dr. Seamon saw visible evidence of a tumor.
A biopsy confirmed: cancer.
“Chris had a tumor that measured 6 centimeters—that’s big—and it had invaded her cervix and involved several lymph nodes,” Dr. Seamon said. “Any time lymph nodes are involved, it gets very concerning. Her uterine cancer was stage 3B, so considered advanced, but grade 1, so less aggressive.”
Facing fear
On Oct. 18, 2016, Dr. Seamon performed a hysterectomy on Chris.
“I loved Dr. Seamon the moment we met,” Chris said. “She exuded confidence, and I thought, ‘I want my life to be in her hands.’ It was my first surgery, so a big deal for me. The cancer didn’t scare me as much as the surgery did.”
Chris had already seen the realities of cancer up close in 2010, when doctors diagnosed her husband, Steve, with non-Hodgkin’s lymphoma.
Her husband had gotten through that. She felt confident she would, too.
“We are strong in our Christian faith,” Chris said. “I knew I would be OK.”
Her new grandson also gave her the strength she needed.
“Grayson was the first face I saw after surgery,” she said. “And he came home the day I got the call I have cancer, so he’s my wellness marker.”
After surgery came the hard work of chemotherapy and radiation treatments at Spectrum Health Lemmen-Holton Cancer Pavilion.
Chris also worked with Spectrum Health nurse practitioner Kelly Conley in Dr. Seamon’s office, who guided her through the treatments.
“I went through chemo treatments in 2016 and radiation treatments in 2017,” Chris said. “The chemo side effects made me feel like this is working. The radiation was harder. I was nauseated each time, so they gave me pills to control the nausea.”
Finding support
Near Thanksgiving 2016, Chris began chemotherapy.
She remembers greeting her sister-in-law around that time and watching as a hunk of her own hair fell onto her sister-in-law’s shoulder.
The following day, Steve shaved Chris’ head.
“Chris had great family support,” Conley said. “And that really helps.”
Chris asked her medical team not to tell her the stage of her cancer. She didn’t want to know. Not until she had beaten the cancer.
By March 2017, Chris felt like her body could no longer rebound from the tough treatments. Her blood platelets weren’t returning after treatment and she began to feel pain on her left side.
“My inner cheerleader was silent,” she said.
She feared a return of the cancer.
“It turned out I had shingles,” she said. “My bone marrow was mad at me. The shingles hurt so much that I couldn’t even wear underwear. I didn’t want anything to touch my skin.”
The treatment had weakened her immune system, opening the way to a shingles infection. She received treatment for that, but doctors then had to cancel the final cancer treatment to let her body recover.
Wellness marker
Nearly three years after the diagnosis, Chris shows no signs of cancer. She credits a great medical team and her support system. And God.
The support system is especially important, she said.
“I started a support group at my church for women experiencing cancer,” Chris said. “We call ourselves The Victors. The group started with four members but is now up to 28. My husband leads a men’s group whose wives are cancer survivors, too.”
Even while undergoing treatments, Chris never missed a chance to watch her grandsons.
“I got so much strength from those boys,” she said. “Little Grayson is now 2 1/2 years old. And that’s how I know how long it’s been since I’ve been cancer-free.”
For the next few years, she’ll continue to have appointments with Conley and Dr. Seamon.
But she’s looking forward to Grayson’s fifth birthday. That’s when she’ll know she has hit an important milestone.
“The first three years have the highest risk of reoccurrence of the cancer,” Dr. Seamon said. “When you reach five years, survival rate is very good.”
Dr. Seamon offered a closing word of awareness: “The most important thing for women to know is to never ignore bleeding outside of a normal menstrual cycle. That includes bleeding after intercourse or ‘just’ spotting after menopause.”



























 /a>
/a>
 /a>
/a>
 /a>
/a>
So happy to hear how well you are doing! Of course one of your best friends my daughter has kept me updated.
You girls grew up together , I always enjoyed your sleepovers!
I am confident you will continue to do well!
You are a Blessing to others!
Lots of Love Chris😘