Sara Riemersma has dedicated her life to saving lives.
The paramedic never thought one of the lives that would need saving would be her own.
Sara, 33, always dreamed of working for an ambulance service. She went to EMT school right after high school and worked as a paramedic from 2005 to 2012.
But as her weight ballooned, her dream burst.
“I had to quit because I weighed too much and could no longer do my job,” the Zeeland, Michigan, resident said. “I weighed almost 400 pounds. I was having difficulty lifting the gurney, I was out of breath, sweating and it was difficult walking. Every day I would be wondering, ‘Am I going to fit behind the steering wheel?’”
The weight not only burdened her body, it burdened her mind. And her soul. In May 2014, she underwent bariatric surgery. Soon thereafter, she underwent gallbladder surgery as well.
Sara turned to opioids to fight the physical and emotional pain following surgery. The pain killers gripped her, and wouldn’t let go. She became addicted.
In October 2014, while on a camping trip with her parents near Allegan, Michigan, the unthinkable happened.
“I overdosed on Norco,” Sara said. “My mom happened to wake up at like 2 in the morning and she found me unresponsive in the trailer. She called 911. My dad (Doug) ended up having to give me CPR. He used to be a firefighter, but the dispatcher did talk him through it.”
Her mom, Karen Riemersma, remembers it well. Too well. The camping trip still haunts her.
“I woke up around 2 a.m. to use the bathroom,” Karen said. “That was not something that happens regularly at that time, so that in itself was a Godsend. I noticed that Sara had fallen asleep on the couch. She never has done that before. I went to wake her to go to her bed. She was completely unresponsive. I shook her, yelled her name, no response.”
Her daughter was gasping for breath, a “very slow grunting/breathing thing,” Karen said, the only sign that her daughter was still alive.
“Everything from here on until the paramedics arrived seemed in my mind to be in slow motion and very vivid,” Karen said.
Paramedics transported Sara to a nearby hospital, where doctors intubated her.
“I had aspirated,” Sara said. “I had vomited and it went into my lungs. They had a hard time with the ventilator because my lungs were really messed up. I was too sick to be there.”
Spectrum Health Aero Med transported Sara to Spectrum Health Butterworth Hospital in Grand Rapids the following morning.
Life-saving measures
“The doctors told my parents, ‘She needs to be on ECMO,’” Sara said.
But given Sara’s medical background, she had already had a talk with her parents a few years prior. She told them she never wanted to be kept alive by machines.
“My mom had a hard time deciding,” Sara said. “But doctors told her, ‘If she doesn’t get put on this, she is going to die.’”
From that early Monday morning until the following Sunday, ECMO sustained Sara’s young life, doing the work that her heart and lungs were unable to do.
“They told my parents, ‘If she makes it through this, we don’t know how her brain is going to react,’” Sara said.
Her Mom remembers the conversation, but only the doctor’s face. Surroundings blurred.
“When the doctor talked to us, it was surreal,” Karen said. “It was kind of like I had tunnel vision. I just focused completely on his face. Weeks later, I asked my husband if there were any other people in that room. He said there were. I could only see the doctor.”
Like a haunting echo, Karen and Doug were familiar with ECMO. A baby from their church was put on an ECMO machine.
“I knew what a big deal it was,” Karen said. “We were told more than once that we were in for a long journey. It was very frightening.”
Greg Marco, MD, a Spectrum Health cardiothoracic critical care specialist, said Sara’s lungs were failing from life-threatening pneumonia.
“Her lungs were unable to provide her body with enough oxygen to function, even with the most sophisticated of conventional therapies,” Dr. Marco said. “Ms. Riemersma was placed on a supportive therapy called ECMO. During this therapy, a patient’s blood is circulated outside the body and is oxygenated by an artificial lung. The blood is then returned to the patient, fully oxygenated, where it can supply enough oxygen to the body to preserve brain, kidney and other organ function.”
Holding onto hope
A mom, a dad, a child. Parents huddled in a hospital room, staring at a child they may lose—if not to death, maybe to brain damage. Nothing worse, perhaps, in the cosmic collection of nightmares.
But fate trips over itself sometimes, and spins a new reality. And the one who saved lives would be destined to go on to save more.
A week and a half later, Sara walked out of the hospital. And left her opioid addiction behind, for good.
“She responded amazingly well and it’s a miracle she is here today,” Karen said. “So many miracles along the way…me waking up at 2 a.m., my husband knowing CPR, the fact that we have Aero Med available and the weather was good for the flight. The fact that Spectrum Health has ECMO is huge. So many things fell in place to make the miracle that Sara is still alive today.
“God was not done with her yet. And she realized it.”
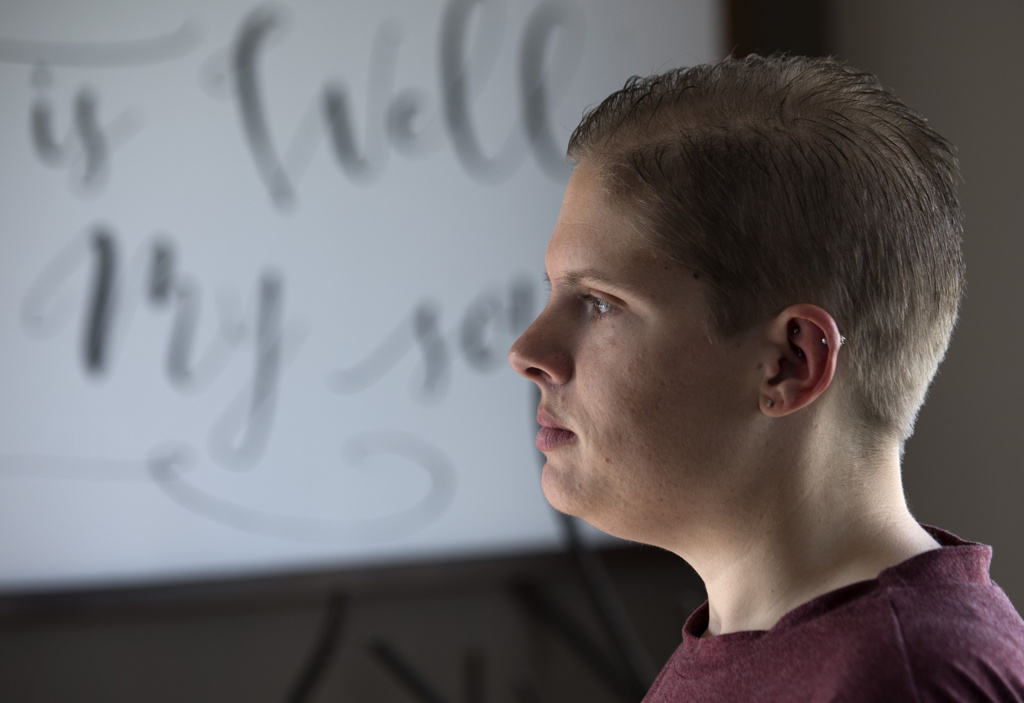
Sitting in the family living room on a recent weekday, while her mom cut hair in their in-home salon, Sara played with her dog, Snickers.
She spoke of her life-long love of the ambulance world, and how she battled back from her addictions and weight issues to start her career all over again. From scratch.
She re-enrolled at Baker College in Muskegon and obtained her EMT credentials again in 2017, a decade after the first time.
“It’s a job I fell in love with,” she said, surrounded by wall and fireplace décor that reads “It is well with my soul” and “Forever and ever amen.”
“I just wanted to do it again,” she said. “It can be very adrenaline-filled. You never know what you’re going into when you go into work. I think that’s one of the things that draws me to it. I can’t sit in an office in front of a computer. I did that in school. I like the unknown.”
Sara also likes the rewards—potentially saving lives. But the little things matter, too.
“A large chunk of our job is little old ladies who have chest pain and shortness of breath,” she said. “I like being there for someone on what is probably the worst day of their lives. If I can put a smile on someone’s face, I’ve done my job.”
Sara said her own near-death experience changed her perspective on her job. And her life.
‘I can relate’
“I think it gives me more of an understanding of what they’re going through and what I need to do for them and what I need to say to them,” she said. “I can relate.”
While scratching Snickers’ back, Sara said she doesn’t have much recollection about her overdose, only stories she’s heard after-the-fact.
“When I did start coming to, I remember having excellent care,” she said. “I’m able to use that situation to help other people. We just had a call very similar to what happened to me. It was a female in her 50s. I’m glad I could do something for her, like someone did for me, and hopefully the outcome is the same.”
Sara realizes her outcome may be an outlier. That she’s blessed to be here, as bleak as things looked that darkest of nights heading into dawn in October 2014.
“I know a lot of people don’t make a full recovery,” Sara said. “I walked out of the hospital 10 days later. It was quite the ordeal to live through.”
As Sara stroked Snickers, a tattoo on her right forearm flashed the words “my story isn’t over yet.” Her left forearm reads “and so I kept living.”
Dr. Marco said her story could have had a much different ending.
“ECMO therapy is available in very few medical centers nationally,” Dr. Marco said. “It is very possible that Ms. Riemersma would not have survived were it not for the availability of this therapy.”















 /a>
/a>
 /a>
/a>
 /a>
/a>
Incredible story. Glad you can continue to help others.
I Know Sara and her family. It is their faith and trust in GOD that lead them thru those dark days. GOD is using Sara to bless others.
Micki, thank you! You are so right. Without God’s love and grace we couldn’t have made it.
Miraculous recovery. Excellent writing. God is good.
Sara, you are a ROCK STAR. Thank you so much for sharing your incredible human story of vulnerability and strength.