By the time Amie Quist reached her mid-30s, she no longer felt like herself.
She underwent a partial hysterectomy at age 25 after a difficult pregnancy that led to the birth of twins at 27 weeks.
“My boys were in the neonatal unit at Spectrum Health, but one of my babies passed away,” Quist said. “Hayden lived, and he wouldn’t have survived without the care he received there. He weighed 2 pounds.”
Today, Hayden is preparing for his wedding. Quist couldn’t be prouder.
Quist gazes out at the cold waters of Lake Michigan. She left Grand Haven for some years, but she returned because the lake drew her back. This is home.
Having worked as a paramedic, but now at the Grand Rapids branch of Ferris State University in pharmaceuticals, Quist understands what good medicine can do. When it came to her own health care, however, she sometimes felt adrift.
“I’m 46 now, and I’ve been going to different providers to find out why I feel like garbage,” she said. “I’ve been treated for depression, but I knew I wasn’t depressed—I’m well-adjusted and in a happy marriage with a good life—but everyone kept treating something else. Oh, it’s your thyroid. Oh, it’s your low iron. Oh, it’s chronic fatigue. I felt like I was losing my mind with all these different diagnoses.”
Getting the whole picture
Quist likes the analogy of the blind men in a room with an elephant. In the ancient Indian parable, one blind man touches the elephant’s foot and likens the animal to a tree trunk. Another touches the trunk and likens the elephant to a thick snake. Yet another touches the elephant’s ear and describes the animal as fan-like.
“It was very frustrating to feel like I was being tossed around from doctor to doctor and put in a bucket with each diagnosis,” Quist said. “Everyone seemed to look at only one symptom at a time.”
Then her new provider suggested Quist visit the Spectrum Health Midlife, Menopause & Sexual Health Clinic, where she met Julie Ondersma, FNP. Ondersma specializes in obstetrics and gynecology and is certified in menopause medicine.
Quist first visited the clinic in November 2019.
“Amie was feeling very frustrated,” Ondersma recalled. “We needed to look at her symptoms as a group. We talked for a long time, so that I could get to know my patient and what’s important to her, what her lifestyle is like.”
Hormones, Ondersma said, can affect everything and Quist’s lab tests showed evidence of hormonal changes.
Ondersma did an inventory of Quist’s lifestyle, noting how much water she drank, her exercise habits, sleep patterns and diet.
Quist already had healthy habits in regard to diet and regular exercise. She typically ran 10 to 15 miles each week, although her distance had recently fallen to 5 miles.
The two talked for nearly an hour.
Different for every woman
Generally speaking, menopause is divided into perimenopause, early menopause, menopause and post-menopause. Hormones fluctuate through all these stages and symptoms include hot flashes, night sweats, weight management issues, decreased sex drive, vaginal dryness, and behavioral and emotional changes. Heart health may also be affected.
“We go by a timeline called STRAW—Stages of Reproductive Aging Workshop,” Ondersma explained. “(The stages of menopause) can take as long as a decade of your life—with the average age of menopause around 51—so that’s why our clinic exists, to help women through all that.”
Quist’s partial hysterectomy may also affect this timeline, as such surgery could expedite menopause. Since she hadn’t experienced hot flashes or night sweats, however, Ondersma ruled out menopause and determined Quist’s symptoms were related to perimenopause changes.
Perimenopause can last anywhere from one to seven years, and hormones may still look normal at that point.
“But a lab test is just a snapshot of one day,” Ondersma said. “We treat people, not numbers.”
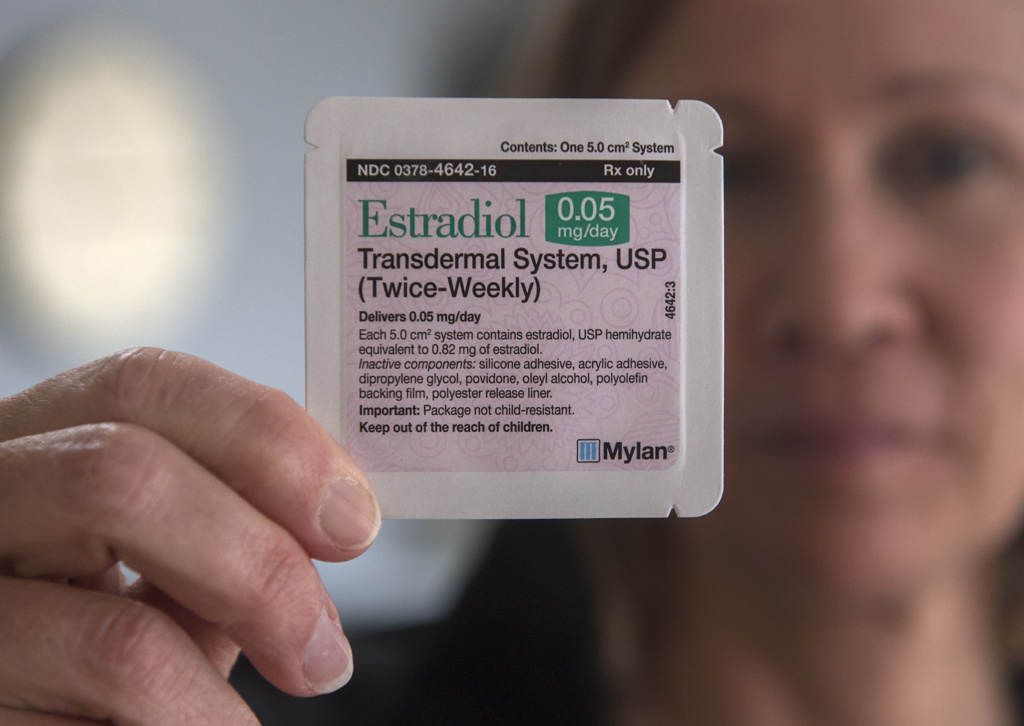
She decided Quist could do well with a low-dose estrogen patch.
“Finally, somebody listened to me and connected the dots,” Quist said. “After four or five months on the patch, wow, I was feeling like myself again.”
Quist felt her energy return bit by bit. By her second visit to the clinic in January 2020, she felt a big difference in her health and well-being.
“When you start feeling better, then you realize just how bad you were feeling before,” she said.
Back on the run
In the past, Quist ran marathons and completed challenging triathlons.
Getting back on the road felt great.
Soon, she even had enough energy to spare to return to school to work on a master’s in public health at Ferris State University.
When Quist felt a slight decline in her well-being, Ondersma made a small adjustment in the dosage of her estrogen patch, and Quist resumed her active lifestyle.
Ondersma said women shouldn’t fear hormone therapy.
The Women’s Health Initiative results 10 years ago scared many women away from using hormone therapy altogether, Ondersma explained.
“We’ve learned a lot since then about the risks and benefits of hormone therapy,” she said. “For most women, experts agree that (it) is recommended to control moderate to severe menopause symptoms, such as hot flashes and vaginal dryness, within 10 years of menopause and up to age 59. Individualization is key in the decision to use hormone therapy. Consideration should be given to the woman’s quality of life priorities as well as her personal risk factors such as age, time since menopause, and her risk of blood clots, heart disease, stroke and breast cancer.”
Quist attested: “Julie and this estrogen patch have given me a new life.”
She is looking forward once again to earning a master’s degree, to a new career, to more marathons and to her son’s wedding.











 /a>
/a>
 /a>
/a>
 /a>
/a>