Ask Mark Erickson to recount what happened to him on the afternoon of July 31, 2020, and he’ll shake his head in near disbelief—even now, more than a year later.
That’s the day Erickson came face to face with his mortality.
He lived to tell the story because the health care system worked, from end to end. And because the right person came by at the right time with the right response.
‘He wasn’t breathing’
That sunny Friday, Erickson, 54, a mortgage underwriter, and his daughter Kayla, 20, a university student, did what they often do at the end of a workday: get outside.
Residents of Comstock Park, Michigan, the two like to hop on the nearby White Pine Trail to go walking, biking or inline skating.
“That’s where we go—‘Hey, let’s go hit the trail.’ ‘OK,’ boom. And off we go,” Erickson said.
This time they grabbed their bikes and headed north toward Rockford.
Seven miles into their ride, where the trail crosses Childsdale Avenue, Erickson blacked out and crashed to the ground, lifeless.
Kayla, cycling ahead of him, sensed his absence. She stopped, saw him lying on the path and tore back, terrified.
A couple driving north on Childsdale happened to see Erickson fall. They pulled over to call 911.
Coming upon the scene a half-minute later, Tyler Nickels followed suit and jumped out of his car.
“My first reaction to seeing him—he was pale gray, basically no color in his face,” Nickels said. “I could tell just the second I got out of the car he wasn’t breathing.”
Nickels, a Spectrum Health clinical data analyst, had an ace up his sleeve. For four years, until just eight months earlier, he’d worked as a nurse in the Spectrum Health Fred and Lena Meijer Heart Center.
He knew what to do for Erickson.
Checking for a pulse and not finding one, he started chest compressions.
When he couldn’t get Erickson breathing after nearly a minute of hands-only CPR, Nickels wanted to supplement chest compressions with rescue breaths.
But this was the summer of 2020, at the height of the coronavirus pandemic—not a good time for mouth-to-mouth resuscitation.
“If it wasn’t for COVID, I probably would have done it myself, but without knowing him and just being a stranger, I asked if there was a family member that could do some breaths.”
Though her father’s collapse had left her frantic and distraught, Kayla stepped up to help.
The two worked together until first responders arrived—first a Rockford police officer, then crews from the Plainfield Township Fire Department, Kent County Sheriff’s Office and Rockford Ambulance.
Stepping back, Nickels had doubts about Erickson’s chance of survival; he didn’t seem to be coming around. But as concerned as he was about the man’s future, he worried even more about how this event would affect Kayla.
Eventually, unable to do more, Nickels and his wife continued on to a brewery around the bend, where they were meeting friends.
There they ran into the couple from the first car, the 911 callers. They’d gotten Kayla’s phone number and agreed to let Nickels know what they learned about Erickson’s status.
Cardiac arrest
Nickels later learned that the paramedics successfully revived Erickson and rushed him to Spectrum Health Butterworth Hospital, where he underwent a series of tests.
According to Araya Negash, DO, the cardiologist on call when Erickson arrived in the trauma bay, EKG testing didn’t show evidence of an acute heart attack. Erickson therefore didn’t need an emergency heart procedure.
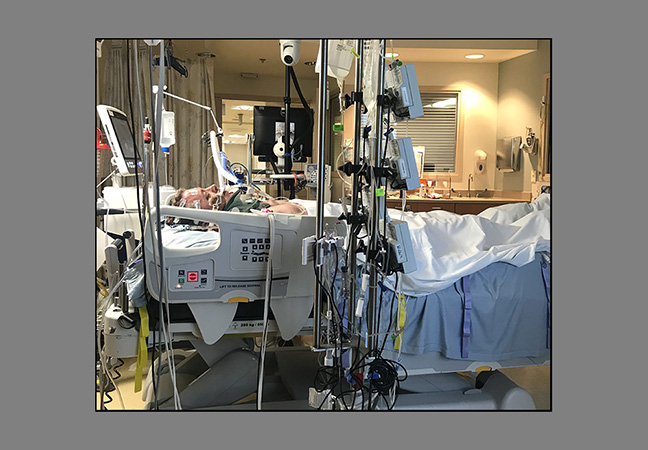
Tests did show bleeding in his brain, likely related to his fall. Erickson received sedation medications and was moved to the ICU for close monitoring and evaluation by the neurosurgery team.
As doctors dialed back his sedation medications, Erickson began to recover.
Further testing showed him to be neurologically intact, Dr. Negash said, and stable enough to undergo heart catheterization to explore the cause of his collapse.
Dr. Negash threaded a catheter through a thin tube inserted in an artery and took pictures of the arteries around Erickson’s heart. The images showed severe coronary artery disease—blockages in several vessels, including the left main coronary artery.
Though Erickson hadn’t experienced heart disease symptoms, these blockages had triggered an irregular heartbeat, or arrhythmia, which led to sudden cardiac arrest.
“A cardiac arrest at its core is an electrical issue, so your heart goes into an arrhythmia that oftentimes is fatal,” Dr. Negash said.
“In this case, it was a blocked artery issue that sparked an electrical issue—ventricular fibrillation.”
Because of the number and location of the blockages, Dr. Negash decided against stenting and called in the cardiothoracic surgery team.
Their evaluation led to a four-vessel bypass surgery, performed by Stephane Leung, MD.
To reduce the risk of a repeat cardiac arrest, Erickson also underwent surgery with Michael Brunner, MD, an electrophysiologist, who placed an implantable cardioverter-defibrillator below his collarbone. The defibrillator will deliver a lifesaving shock if Erickson develops another lethally fast heart rate.
Perfect timing
During his recovery, Erickson received a visit one day from a nurse who had heard Nickels’ story about the White Pine Trail rescue. In talking with a colleague, she’d matched Erickson to the story.
This nurse was Nickels’ mother-in-law, a longtime staff member at Fred and Lena Meijer Heart Center.
“So she walked into his room one day and said, ‘Hey, you may not know me, but I know you,’” Nickels said. “‘My son-in-law actually was the one that did compressions when you collapsed on the bike trail.’”
Eager to express his gratitude, Erickson asked for Nickels’ phone number. The two men have been in communication ever since—initially by text, then by phone and more recently in person.
“The whole thing just makes my head spin—just thinking about all the things that fell into place perfectly and how the Good Lord put everyone in my life like that,” Erickson said.
He still chokes up thinking about the way events unfolded that day.
“(Tyler) was everything to me, he really was. CPR doesn’t start up, and I’m not here, honestly. … As I told him, ‘You had to be the perfect person in the perfect spot at the perfect time for me to be here.’”
Kayla’s role in his rescue also sparks powerful emotions.
“She stepped up and was a true hero,” he said. “I just can’t imagine putting my child through that. But she did it. … She’s just been amazing through the whole thing.”
Erickson’s ability to work through his emotions has contributed to his strong recovery.
“He’s processed this whole event in a very healthy way,” Dr. Negash said. “He’s really kind of taken to the emotional part of getting better a lot faster than most of my patients—men and women.”
Erickson’s physical recovery has taken a fast track, too.
“When he walked in the clinic the first time I saw him back, I was expecting a very different person. If you saw him in the waiting room, you would assume that he was driving somebody else to their appointment. … I didn’t expect him to come in bright-eyed and bushy-tailed, with no real complaints.”
Erickson tells a similar story. His physical therapists had to develop a custom training regimen to keep him challenged.
And throughout his 23-day hospital stay, staff regularly told him his appearance didn’t match the things reported in his medical chart.
“I’m like, ‘I don’t know what that means. … Everyone keeps coming in and saying I don’t look like my chart. Is this good or bad?’ And they looked at me and they go, ‘Oh, it’s good.’”
His story, Erickson said, is a tale of perfect timing, of selfless heroes, of faithful family members and of “phenomenal” medical staff, all along the way.
“I couldn’t have been placed in better hands.”

























 /a>
/a>
 /a>
/a>
 /a>
/a>
NICE JOB TYLER!!!!!!
Amazing story! Amazing heroes!
Mark is one of my best friend’s brother. I got a call from her, when she was in another hospital recovering from an invasive surgery she had to go through. The first thing she said to me was, Kathy, don’t freak out. Then she told me what happened. I was in shock but didn’t freak out because she asked me not to. I was already really concerned about her surgery and recovery.
Thank God for putting all of these heroes in the right place at the right time. God bless everyone who helped him out to save his life. 🙏🏻🙏🏻🙏🏻