At age 21, Ben Krieger’s weight jumped 30 pounds in a summer before dropping quickly back to normal.
He seemed tired all the time. And thirsty. So thirsty, he downed a 24-pack of water every day.
As a college student with a busy job and a new baby, he blamed it on stress. Even his mom, Sue Krieger, thought it looked like typical college-age behavior.
But looks can be deceiving.
Ben had grown sick. He just didn’t know it.
On Sept. 4, 2013, he became violently ill and began vomiting profusely. When he grew lightheaded and could barely walk, his girlfriend rushed him to the emergency room at Spectrum Health Butterworth Hospital.
“On the way, I was going in and out of consciousness,” Ben said. “They asked a list of questions, but I don’t remember a thing of it.”
It didn’t take long for doctors to diagnose Ben with Type 1 diabetes. It has also been known as juvenile diabetes, although that terminology is obsolete because Type 1 diabetes can develop at any age—a fact that takes many people by surprise.
Outside the zone
Ben and Sue now have 20/20 hindsight.
“Looking back, how do you go through that much water?” Ben said. “I had this nonstop thirst.”
“When he started putting on weight that summer, I saw the pizza boxes and knew he was eating junk food, but it didn’t mean a thing to me,” Sue said. “Then, to drop a lot of weight, like 30 pounds, in a couple of weeks. That should have been a sign … how could I miss that?”
“I thought we were in the safety zone,” Sue said. “He’s a young adult.”
Ben exhibited the classic symptoms of diabetes, according Gregory Deines, DO, a specialist in diabetes and endocrinology with Spectrum Health Medical Group.
These symptoms include extreme thirst, unexplained weight loss, fatigue and ravenous hunger.
The difference between typical college-age behavior and diabetes symptoms? The extremes, Dr. Deines said.
“Unfortunately, the symptoms can be attributed to other things and sometimes people wait too long,” the doctor said. “Once the symptoms start snowballing, a patient can get very sick very fast.”
In Ben’s case, it became a life-threatening situation.
“My blood sugar was 978, which is almost unheard of,” Ben said.
He almost slipped into a diabetic coma and his organs began to shut down.
“It came out of nowhere and got to the point where it was almost too late,” Ben said. “It’s a scary situation … very, very scary when you don’t have any idea what’s going on with your body.”
‘Diabetic denial’
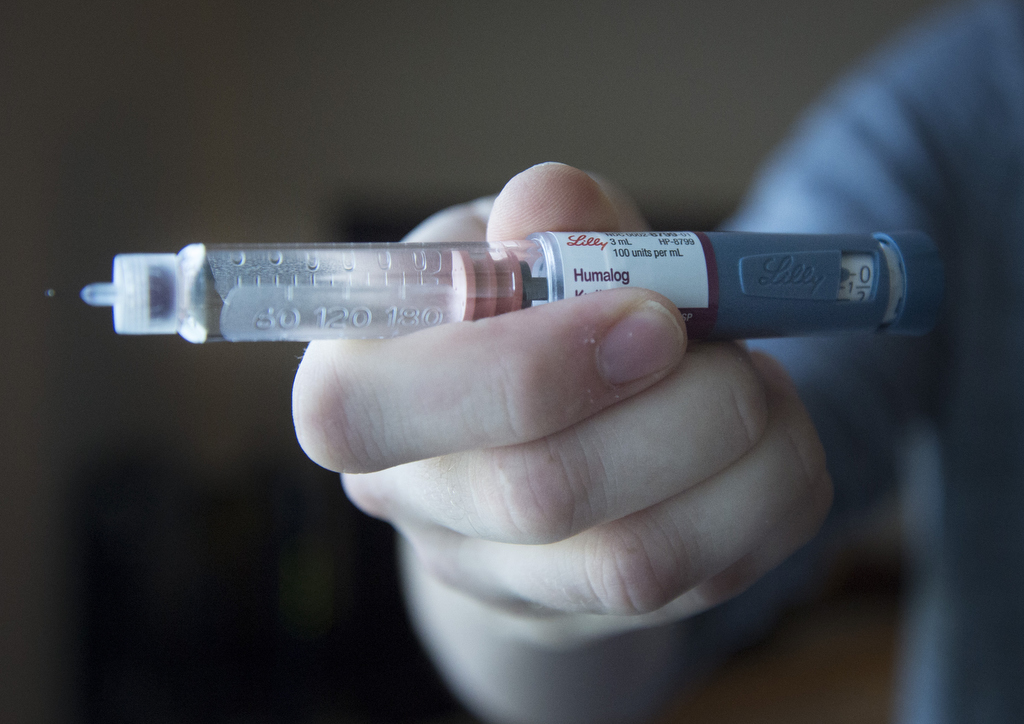
Patients with Type 1 diabetes can live normal lives. But because their bodies don’t make insulin naturally, they must monitor their blood sugar and inject insulin throughout the day to avoid severe complications such as kidney damage, blindness, heart attack and stroke.
It’s not easy.
As Ben likes to say, he initially found himself in a state of “diabetic denial.” He now knows he needs to stay healthy, not just for himself but also for his 4-year-old son, Logen.
Ben also overcame his aversion to needles, so that he can now give himself insulin injections. He counts carbs, too, and eats lots of proteins and veggies.
Because there can be a genetic factor, he’s also keeping a close eye on little Logen, who understands that daddy needs shots. Logen is also fascinated by watching the injections, although he grows concerned if there’s too much bleeding.
Unlike Type 2 diabetes, which can be linked to obesity, high blood pressure and high cholesterol, Type 1 diabetes appears to be an autoimmune issue that prevents the body from creating insulin.
Ben’s experience has been an eye-opener for his entire family.
In fact, when his younger sister in Montana developed Type 1 diabetes a year ago, she recognized it quickly.
“Type 1 diabetes can happen to any person at any age,” Dr. Deines said. “If someone has any of the classic symptoms, they should see a doctor sooner rather than later.”















 /a>
/a>
 /a>
/a>
 /a>
/a>
Thank you for this story which gives more awareness to the symptoms of diabetes. My Dad, at the age of 49, was rushed to a small country hospital with the onset of type 2 diabetes in 1987 with a blood sugar over 1400! (yes, 1400) He staggered out of the emergency room, went home, and returned for care (at the plea of his family). Changes in lifestyle, healthy eating habits and sure determination are a testimony that accumulative medical conditions of heart attack, stroke, diabetes, COPD, and congestive heart failure can be managed.
Wow, what a story. So glad your dad returned for care. Thank you for sharing and for your kind comments! 🙂
As an older man that ignored the symptoms of Diabetes that I should have recognized due to my prior experience with diabetes. I too was close to death before I went into the ER. My A1C was 13+. I to was thirsty all the time and lost a great amount of weight. My pain doctor spotted the weight loss but before I could get into my primary care doctor I went to the ER with my sons insistence.
Having cared for a brittle diabetic mother for 30 years before she passed I knew that I needed to toe the line, which I did. I measured or weighed every thing I ate to figure out the carb content. Counting carb helped me control my blood sugars by adjusting the insulin dosage to carb intake.
I am Dr. Deines’s odd ball diabetic as my pancreas started making insulin again so that for a while I was off all insulin. I am now classed type 2 and am on metformin.
I can not thank Dr. Deines and his group enough for the fine treatment that I have received.
Thank you for sharing your story, Tom, and for your kind words. You’re an inspiration.