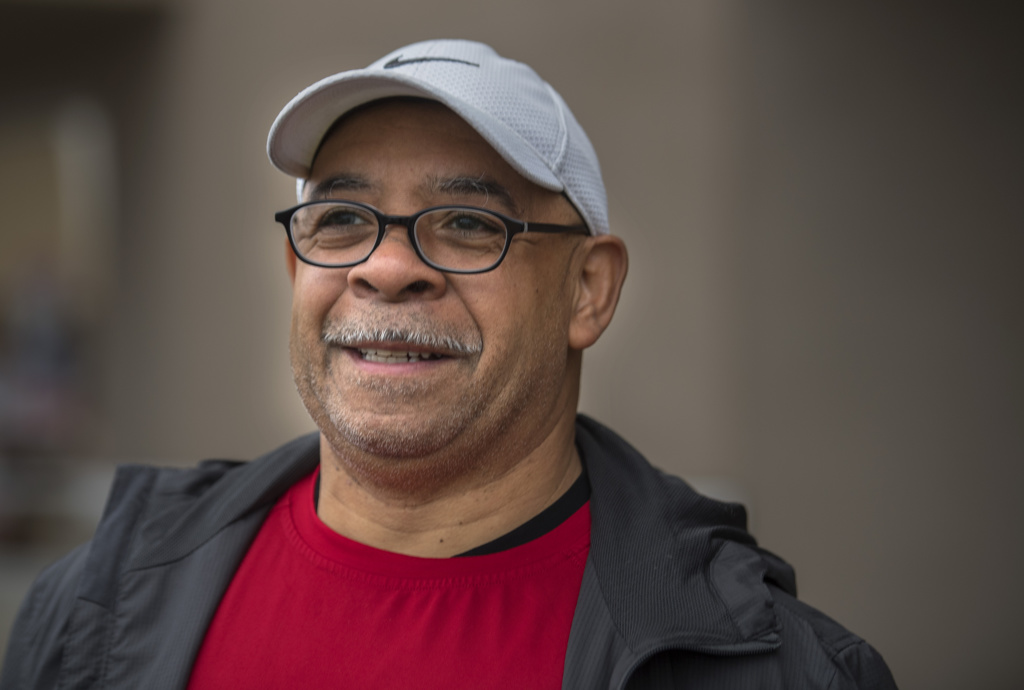
Wallace Isaac Gaunichaux, 60, is no couch potato.
The Wyoming, Michigan, resident has long trained to participate in marathons and triathlons—even the Ironman race, known for its grueling endurance test of swimming, bicycling and long-distance running.
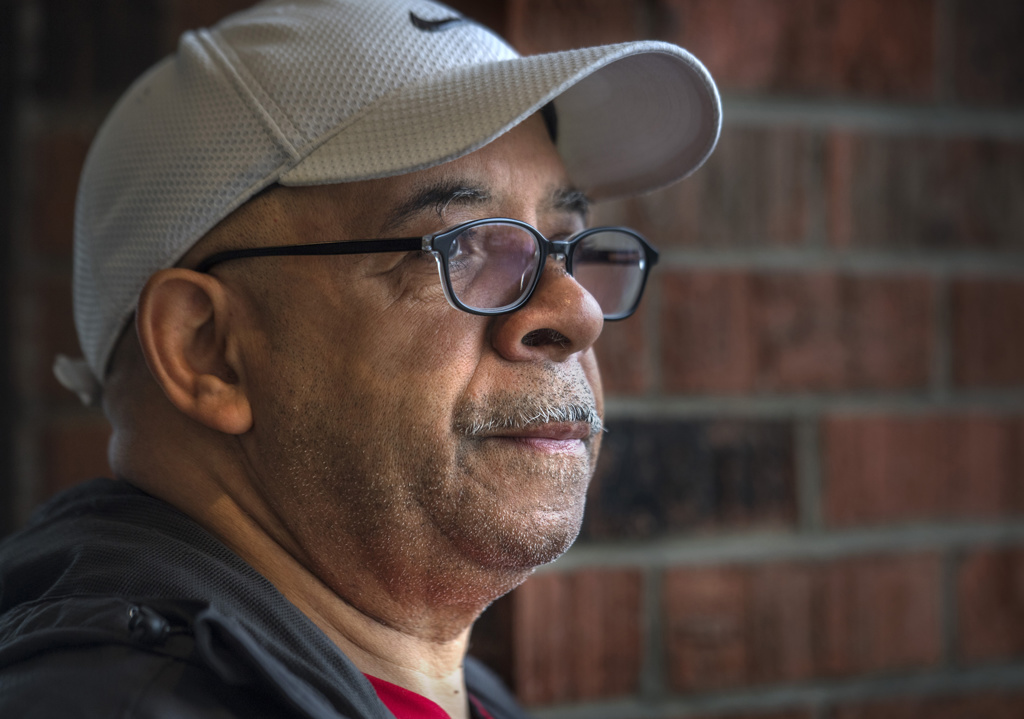
In 2010, leg pain brought Gaunichaux to a screeching halt.
“My leg was swollen and painful,” he said. “I went to see one doctor after another at one hospital after another, but no one seemed to be able to fix it.”
Doctors soon diagnosed Gaunichaux with May-Thurner syndrome, also known as iliac vein compression syndrome.
Symptoms can include soreness and swelling, changes in skin color to a red or purple shade, a feeling of heaviness in the leg and tenderness or throbbing. Veins may also begin to look enlarged.
“May-Thurner syndrome affects the two main blood vessels, the vein and the artery, that go into the legs,” said Jennifer Watson, MD, RVPI, Spectrum Health Vein Center site lead and vascular surgeon. “The right iliac artery can sometimes rest on top of the left iliac vein in the pelvis and cause pressure.”
As Gaunichaux began to confront his condition, he grew frustrated at the lack of answers out there.
“Doctors just kept giving me blood thinners like Coumadin and telling me to wear compression socks,” Gaunichaux said. “But the problem was just getting worse. I wanted a true second opinion, not just to be sent to another doctor in the same office.”
In August 2019, his quest for substantive answers led him to one place.
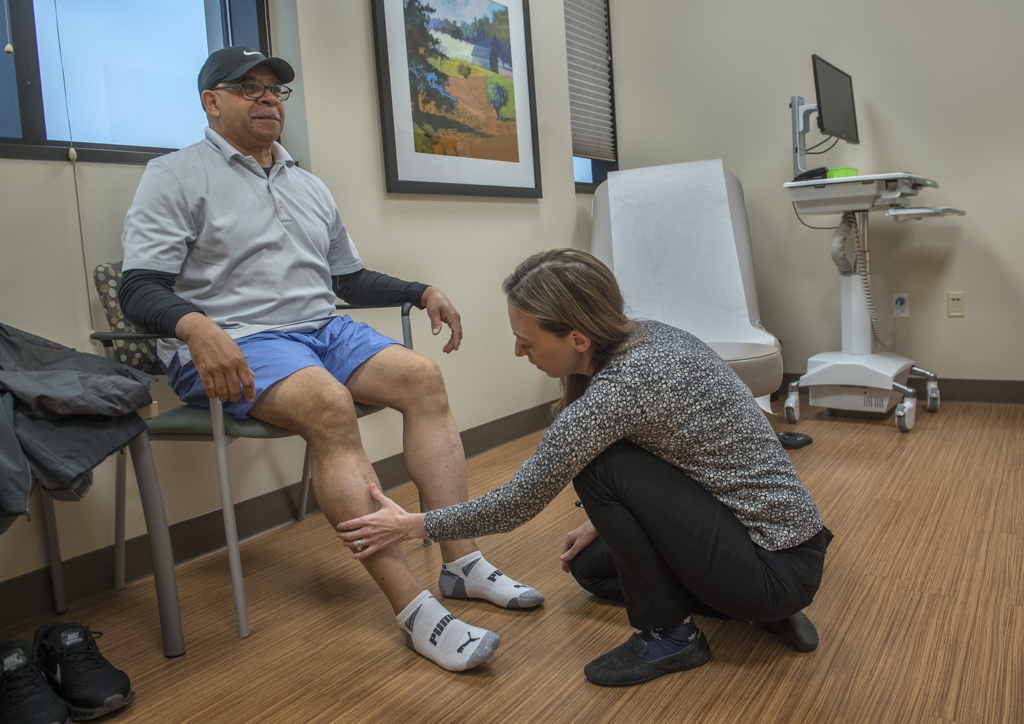
“That’s when I was referred to the Spectrum Health Vein Center and met Dr. Watson,” he said.
Long-awaited help
Dr. Watson performed an ultrasound on Gaunichaux’s legs and found several clots. She also conducted a CT scan to gain more detail.
“Blood clots can be life-threatening,” Dr. Watson said. “May-Thurner syndrome means you are more likely to have deep vein thrombosis, or DVT, a dangerous blood clot. Arteries move blood away from the heart, and veins move the blood back.
“With May-Thurner syndrome, the right iliac artery squeezes the left iliac vein where they cross each other in the pelvis,” she said. “And that can prevent free blood flow.”
Sometimes, the pinched veins become scarred by the added pressure and it forms a blockage, the doctor explained.
After examining Gaunichaux’s ultrasound and CT scan results and finding both acute and chronic occlusions, Dr. Watson called in Michael Knox, MD, an interventional radiologist with Advanced Radiology Services in Grand Rapids.
Collaboration of experts
Gaunichaux’s treatment would involve a team effort.
First, Dr. Watson.
“When she called me and told me I would be admitted to Spectrum Health Butterworth Hospital, I was ready,” Gaunichaux said. “Dr. Watson explained exactly what would be done—and I knew I had found the right doctor and the right place.”
“Blood clots are one of the leading causes of death in the younger population,” Dr. Watson said.
According to the Centers for Disease Control and Prevention, 60,000 to 100,000 people die from deep vein thrombosis each year and 10 to 30% of these Americans die within a month of diagnosis, she said.
“At Butterworth Hospital, we hooked Wallace up to a machine that ran Heparin, which is an anticoagulant, through his blood to dissolve the clots,” she said.
Dr. Watson also talked to Gaunichaux about placement of stents.
Dr. Knox then took his turn.
“In the interventional radiology suite, I performed leg venograms,” Dr. Knox said. “Catheters were placed from veins behind both knees and contrast dye injections showed a chronic occlusion of the right iliac vein with malpositioned left iliac vein stent from a remote procedure. A small amount of acute clot was cleared and the right iliac vein occlusion was able to be opened with a stent. The malpositioned left iliac stent was fixed with an additional stent on that side.”
He placed stents in the cleared veins.
Soon after, Gaunichaux’s condition began to improve.
“I was in the intensive care unit for a couple days and I watched my legs to see if the swelling would come back,” he said. “It didn’t.”
Back in the race
A month later, Dr. Watson performed another ultrasound on Gaunichaux’s legs.
His blood flowed well through his veins and arteries.
“At work, I’m on my feet all day,” Gaunichaux said. “And I was a little nervous about that. I brought compression socks along, just in case. But I’ve never needed them.”
He’s already on the mend.
“I walk a half-mile to and from work,” he said. “I spend a half-hour on my spin cycle. I don’t want to go too fast too soon, but I plan to work up from walking to running again.”
In fact, Gaunichaux said he has made a resolution.
“I plan to run the Resolution Run around Reeds Lake in Grand Rapids,” he said. “It happens on New Year’s Day 2020, and it’s 4 miles around the lake.”
He’s leaving the compression socks at home.















 /a>
/a>
 /a>
/a>
 /a>
/a>