How do you know if you’re a walking time bomb? Would you know if an aneurysm lurked in your brain, tick-tocking toward a potentially fatal explosion?
Paul Mazaris, MD, a Spectrum Health Medical Group neurosurgeon, chatted with Health Beat about the risk factors for aneurysms and how to determine if you’re among the 1 in 50 who have an unruptured brain aneurysm.
Q: Is there any way to know if you have a hidden aneurysm?
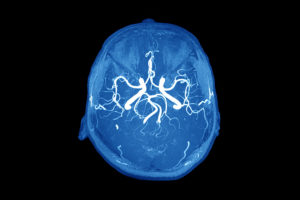
A: No one knows. The only way to really know is to get a screening if you’re concerned. An MRA of the brain. Generally the best indicators are a clinical history. People generally know if they have a family history. You’re at increased risk if you have two first-degree relatives with a history of intracranial aneurysm. When you hear the word ‘aneurysm’ red lights go off. They can be catastrophic. There are only two ways you know if you have an aneurysm. One, if it’s large enough to cause pressure on the brain and cause symptoms like double vision, facial drooping or numbness. The second way to know, if it ruptures, you know it ruptured because it’s the worst headache of your life. The textbook term is a thunderclap headache. Acute onset. It’s like a bomb went off in your head.
Q: Are frequent headaches or migraines a potential warning sign?
A: People who have a history of migraines aren’t at risk for aneurysms. People who have frequent headaches are not at increased risk.
Q: What are the risk factors?
A: If anyone in the immediate family has had an aneurysm, you should have a screening. Family history is the most important. Also, smoking. I tell my patients usually people who have an aneurysm are smokers, more so than not. I tell them that smoking is a risk factor you can control. A lot of patients have a small enough aneurysm (that) we just watch them. I tell them if they continue to smoke, it will get bigger and possibly rupture. The other two common risk factors are high blood pressure that is uncontrolled and drugs that increase blood pressure, specifically cocaine and methamphetamines. Other things are age—anyone over 40—or women. It’s 3 to 2, women versus men.
Q: Is there anything people can do to help ward off aneurysms?
A: Essentially, it’s just healthy living. Good diet and exercise. The things you can’t control, you can’t control (like genetics). It’s like the rule of life. Anything that’s good for you is the most difficult. No drinking, no smoking, no drugs. Excessive alcohol is known to be associated with ruptures. I mean extreme alcohol intake. Social drinking no.
Q: How do you know if you’re in trouble?
A: It feels like a thunder clap headache, like a bomb went off in your head. That’s the most common symptom. The worst headache of your life. You may experience double vision, numbness or weakness in the face. Call 911 immediately.
Q: What are the survival rates?
A: Generally, a third of people who have an aneurysm that ruptures, they don’t make it to the hospital. They die. The other two-thirds, one-third of those have neurological deficits. The other one-third are at baseline and don’t have noticeable deficits. It’s such a catastrophic illness—one-third who have a rupture don’t survive. Two-thirds are dead or have deficits, ranging from mild to severe.
Q: How common are aneurysms?
A: Not very common. It’s not as prevalent as heart disease or cancer or stroke, but it’s extremely dangerous. People should at least be aware of the warning signs. Usually people who have strokes don’t have headaches. About 1 in 50 people has an unruptured aneurysm—3 to 5 percent of the population.
Q: What are the treatment options?
A: Nowadays, with technology, they are being treated with a catheter through the leg after they rupture. Twenty years ago, everyone went into the operating room (for brain surgery). I do open surgery and endovascular. We start in the right groin with a little catheter about the size of a piece of spaghetti. It goes up into the brain to the aneurysm. There’s less morbidity because you’re not making an incision in the head. The catheter is like the straw. Then you take a thread of platinum. When you push it out (through the catheter) it forms a ball. You’re filling that ball in the aneurysm. The blood will start to clot. It turns into a scar and scars off. We used to put a titanium clip on like a clothespin. That’s more invasive.
 /a>
/a>
 /a>
/a>
 /a>
/a>
My close friend had symptoms that dr’s. Thought were heart related …doing all kinds of cardiac testing……..until he had the mother of all headaches……..his aneurysm was near the Circle of Willis. His aneurysm was was noted to be giant. And was coiled over a period of 7 or 8 years for a total of 28 coils as they would become compressed over time…. Eventually they placed a sealant over the opening. Most grateful for the Doc’s at Riverside Methodist Hospital.