These days, Ally Woodhouse’s life looks more and more like that of any other 17-year-old.
She loves hanging with her friends. Goofing around with her standard poodle, Augie. Posting videos on YouTube.
And thanks to Trikafta, the drug she started over a year ago, she sounds more like other teens.
Ally has cystic fibrosis, a progressive genetic disease that causes persistent lung infections and, over time, limits the ability to breathe. It also affects enzymes in the pancreas, as well as sweat.
For the first 16 years of her life, that translated to frequent hospitalizations, home infusions and constant coughing to loosen the thick phlegm that clogged her airways.
Ally also has pancreatic insufficiency. She’s had significant liver issues related to cystic fibrosis and she continues to get her nutrition through a gastrostomy tube.
“Coughing was just a huge part of my life before,” she said. “The worst was that almost every time I laughed, I’d start coughing and not be able to stop. I’d have multiple coughing fits throughout the day.”
She took her first dose of the drug on Dec. 30, 2019. It’s a combination of three different medications that target the protein made by the defective gene.
“By New Year’s Eve, I’d noticed a difference,” she said. “I was coughing less.”
Paula, her mom, said it took her a little longer.
“I was washing dishes one night and thought to myself, ‘I haven’t heard Ally cough today. Hmm. I don’t think I’ve heard her cough all week.'”
Paula dashed into the living room.
“Yep,” Ally said. “It’s the Trikafta. I’m hardly coughing at all.”
“Since then, I’ve only heard her cough about five times in the last year,” Paula said. “She also hasn’t been hospitalized since she started taking it, and her lung function is fantastic. We had no idea just how big an improvement this medication would be, not just for Ally but for the whole family.”
Help for 90%
It’s hard for everyone who loves Ally—her mom, her dad, Rob, her big sister, Kira, a student at the University of Michigan, and her Spectrum Health care team—to fathom just how far she has come.
“Ally was one of the sickest babies that I have ever cared for,” said Susan Millard, MD, a pediatric pulmonologist at Spectrum Health.
Dr. Millard is also the principal investigator for the Spectrum Health Cystic Fibrosis Care Center, participating in cystic fibrosis medication studies for over 10 years.
Cystic fibrosis is caused by at least five or six categories of gene mutations, she said.
These lead to defects in a protein called the cystic fibrosis transmembrane conductance regulator, or CFTR. Because they don’t work the way they should, chloride ions can’t move in or out of cells as they should. That causes thick, sticky mucus to build up in organs, including the lungs and digestive system.
In 2012, Kalydeco, the first drug in the category, was approved for kids 12 and older.
“And it worked great, but only on one specific mutation,” Dr. Millard said. That means it only helped about 3% to 5% of patients with cystic fibrosis.
Next came Orkambi, approved in 2015 for that same age group.
“But it didn’t work as well,” the doctor said. Nor did it have much of an impact on the sweat test for patients with cystic fibrosis. The sweat test measures the level of chloride the body is producing.
“But it was available and eventually approved for kids in elementary school, so that was somewhat helpful for some patients,” Dr. Millard said.
The game-changing news came when Trikafta, the first triple-combination therapy, received FDA approval in 2019.
“Not only is it effective on about 90% of the people with CF, it works really well and fast, with most people feeling better within two weeks,” Dr. Millard said.
She hopes the medication will soon be approved for much younger kids. Studies are underway in children as young as 2.
And for the remaining 10%? There is exciting research underway using CRISPR-Cas9, a genome-editing tool that is faster and more accurate than previous techniques of editing DNA, Dr. Millard said.
These new medications have radically changed the prospect for patients with cystic fibrosis, reducing the number of infections.
Short term, these patients are staying healthier.
“We do not see as many hospital admissions,” the doctor said.
Longer-term? Their extended life expectancy is changing everything about the way patients and their families face the future.
“We’ve been to many funerals,” she said. “The life expectancy with CF used to be in the 20s. Now, it’s in the mid-40s. But with Trikafta, we think people will do much better.”
These improved drugs mean that when babies are born with cystic fibrosis today, “we believe they will have the same life expectancy as anyone else,” Dr. Millard said.
‘My Cystic Fibrosis Life’
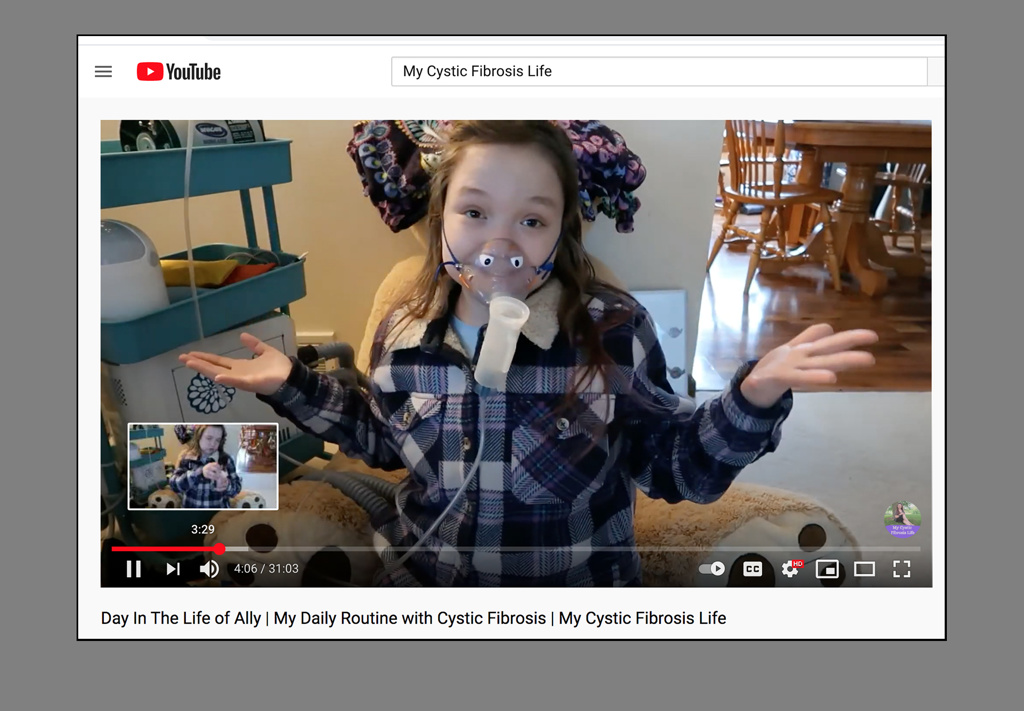
Ally shares her experience with others often, both through Instagram and her YouTube channel, called “My Cystic Fibrosis Life,” where she talks about everything from recipes to Q&As about cystic fibrosis.
With her down-to-earth candor, she keeps it real, detailing the drag of dealing with hours of treatment every day, including using a nebulizer, an oscillating vest and prepping her gastrostomy tube feeds.
They’ve become such a grind she can do much of it blindfolded, something else she’s demonstrated on social media.
And she doesn’t sugarcoat the harsh realities of her diagnosis.
“Trikafta is not a cure,” she wrote in an Instagram post celebrating her first “Trilaftaversary.” (She even made a cake.)
“I still have cystic fibrosis and the other complications that come with it, including my liver and digestive symptoms,” she said.
Still, she marvels at the relief from relentless coughing.
“What these two pills have done for me is absolutely unbelievable,” she said. “I am forever grateful!”
Her family said the medication has moved her to a new level of independence, a step that’s essential for adolescent patients, said Jessica Bustraan, a Spectrum Health medical social worker.
Cystic fibrosis is a challenging diagnosis, Bustraan said. The physical benefits of Trikafta pay off in other ways.
“Teens are trying hard to blend in with peers, which is rough with a constant cough,” Bustraan said. “Plus, nighttime coughing makes it harder to get sleep, which teens really need.”
And because they miss fewer school days, they’re less likely to struggle academically.
“Ally is a unique, spunky girl,” she said. “And it’s great to see that on this medication, she bounces back faster and has more energy.”
At home, her family says that in many ways she is still the same Ally, whether she’s whipping up hot chocolate, lemon whippersnapper cookies or chicken wings.
“She has always been a fun kid to have around,” Paula said. “But it was hard. She was typically in the hospital a few times a year. She struggled with breathing and coughing. It was always kind of a gamble what the day would be like. Trikafta has changed so much for our family.”
Ally isn’t just eager to see better medicines. She’s actively working for them. Besides fundraising for the Cystic Fibrosis Foundation, including raffling off some of her finest cookies, she’s also participating in research.
She’s involved in a study to see if it’s safe for some patients with cystic fibrosis to stop taking some of their inhaled medications if they’re also taking Trikafta.
She thinks of herself as a chronic illness warrior and doesn’t mind doing a little crusading on behalf of people with cystic fibrosis or other conditions.
In one video, she offers a primer for what not to do, including helping others without asking, talking down to them or judging their physical condition based on appearance.
“I am a normal person,” she said. “I can do what everyone else can.”





















 /a>
/a>
 /a>
/a>
 /a>
/a>
I’m a home healthcare nurse. I have had 2 patients with CF in the last 18+ months on Trikafta. Both of them I was seeing for another reason and neither took inhaled meds. It was life changing for both. Both were close to 30, one was disabled and the other was still working.
We are so excited for Ally and her prognosis. All of this continues to give reason and hope to those with the disease and continues to motivate those that raise funds for a cure.
I am glad to read that Ally is doing better. I haven’t heard anything for a loooong time. Love ya 😘