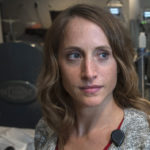
When the sore first started on the bottom of her heel, Cindy Ockert didn’t notice.
Like many people with diabetes-related neuropathy, she often can’t feel anything in her feet.
“I was resting on my daughter’s couch and she noticed it,” Ockert said.
Ockert, 64, sought treatment.
The initial prognosis seemed dire—doctors suspected they might have to remove the lower portion of her leg.
Amputations are often the eventual treatment. About 85% of these types of procedures stem from foot ulcers that won’t heal.
For more help, Ockert then turned to wound care specialists at Spectrum Health United Hospital in Greenville, Michigan.
There she met Drue Orwig, DO, a specialist in wound care and undersea and hyperbaric medicine.
Dr. Orwig believed that Ockert’s wound could be healed—and that her leg could be saved. But it would require teamwork.
“She needed a multi-disciplinary approach,” Dr. Orwig said.
At this point, Cindy went in-patient at Spectrum Health Butterworth Hospital to get care from podiatry, wound and vascular team to help salvage her foot.
From there, she transferred to a skilled facility in Greenville. The Spectrum Health team focused on “offloading”—making sure Ockert wasn’t putting any weight or pressure on the injury at all.
At that point, her wound had grown to cover almost her entire heel.
Patients who put weight or pressure on an injury can get caught in a vicious cycle of partial healing, followed by re-injury.
Next, doctors treated Ockert with a “wound VAC,” or vacuum-assisted closure to promote wound healing. The technique uses a device that remains attached to the injury area, creating a steady negative pressure to stimulate new blood vessel growth.
It expedites healing, particularly in deeper and larger wounds.
After that they began a series of treatments involving skin substitutes, Dr. Orwig said.
“These are a little like skin grafts,” she said. “But instead of using your own body’s tissue, you use other tissues, sometimes animal-based products.”
Ockert, who has lived in a care center for almost a year, has undergone these ultra-modern treatments in Greenville, Michigan, close to home.
“Her (case) is the epitome of a limb-salvage case,” Dr. Orwig said. “She was such a pleasure to care for and it was great to be able to keep her care close to home.”
Deep dive
Wound VACs and offloading aren’t the only tools Dr. Orwig uses to treat patients. She specializes in hyperbaric medicine, which can also be used in treating stubborn wounds, as well as a variety of other medical conditions.
Her interest in hyperbaric medicine started underwater. She’s a devoted scuba diver, an escape that has let her explore deep waters in Hawaii, the Caribbean and an especially magical spot called the Blue Hole of Belize.
She initially trained as a physician in emergency medicine, then shadowed a hyperbaric and undersea medicine specialist. She found herself hooked.
“It was so interesting that I decided to get a fellowship,” she said.
It’s been gratifying to see how diving science, her passion, serves also as a tool for patient care.
Ockert’s success on her healing path also comes down to a great attitude, Dr. Orwig said.
“She was so compliant,” Dr. Orwig said. “Heel ulcers are at very high risk for failure. But because she was so good about not walking on it, we could use the latest and greatest modalities, expediting the wound healing.”
She is now outfitted with special shoes from a local orthotics store.
Ockert describes the wound as about 95% better. She said it won’t be long until she leaves the care facility and moves in with her daughter in Ionia.
She’s spent a lot of time playing with the family dog, working crossword puzzles and gradually regaining mobility.
All four of her daughters live nearby, along with several grandchildren and great-grandchildren. She said she’s looking forward to hugging them all again when she leaves the care center.
“It’s been a long haul,” she said. “I’ll be glad to get home.”











 /a>
/a>
 /a>
/a>
 /a>
/a>