Happy news came to the Christensen family on May 3, 1990: “You have a baby boy.”
Just two hours later, doctors took the newborn, Andrew Christensen, into surgery.
A week or so later, he underwent a second surgery.
By his third surgery, in second grade, that little boy became fully aware he had a problem.
Andrew Christensen, now 30 and a resident of Greenville, Michigan, came into this world with a congenital cardiac malformation called truncus arteriosus. It’s uncommon, occurring in 0.6 to 1.4 live births out of 10,000.
Stephen Cook, MD, director of the adult congenital heart disease program at Spectrum Health Helen DeVos Children’s Hospital, has been treating Christensen since May 2019.
“When a person has truncus arteriosus, there is only one large vessel, instead of two separate ones to carry blood to the lungs and body,” Dr. Cook said. “With only one artery, there is no specific path to the lungs for oxygen before returning to the heart to deliver oxygen to the body.”
Christensen underwent his fifth open heart surgery on July 23, 2020, at the Spectrum Health Fred and Lena Meijer Heart Center.
Christensen acknowledges it has been a blessing getting to this point.
“I feel great,” he said. “And I hope that was the last open-heart surgery I’ll need, although I know I have to return every year to check up on things.”
First years
During childhood, his heart defect had a way of making itself known on a regular basis.
“When I was 8 years old, I had a stent put in and an aorta that I believe was from a pig’s heart valve,” he said.
He was a tall kid—he’s now a 6-foot-2 adult—and he enjoyed getting involved in sports.
But by the time he reached middle school, he once again felt his body slow down.
“I was pretty bummed,” he said. “I couldn’t skateboard all that summer. Couldn’t hang out with my friends.
“I was in sixth or seventh grade and they had to expand the valve in my heart, balloon it,” he said. “And then I had to relax all summer.”
In 2008, as a 17-year-old high school junior, he wanted to try out for the basketball team.
He had the height and the skills.
While running a drill during practice, he felt his heart hammer more than it should. It felt like his chest might blow apart.
Instead of finding a place on the basketball team, he found himself in a hospital emergency department.
Doctors told him he experienced tachycardia, a heartbeat faster than 100 beats per minute. His had been beating 300 times per minute.
Doctors stopped his heart and restarted it again at a normal rhythm.
But he would need more than that and his parents took him to Ann Arbor for surgery.
“The aorta had stopped working,” Christensen said. “They did surgery on me again and put in a cardiac defibrillator. I don’t ever want to experience tachycardia again.”
A pause between beats
In his mid-20s, life eased and began to move at a normal pace.
He maintained an active lifestyle, enjoying outdoor hiking, camping and biking.
“And I loved going up north, visiting a friend who has a cabin there,” he said.
He attended Northern Michigan University in Marquette for a bit, majoring in communications and broadcasting.
“I’d like to return to that someday and finish,” he said.
Then lightning hit.
Or at least it felt like lightning.
“About five years ago, the defibrillator went off in my chest while I was walking,” he said. “It jolted me, felt very strange, like a lightning bolt coming through my head.”
Christensen’s doctor had retired, so he called a new doctor.
That’s when he met Dr. Cook at Spectrum Health.
“There are three different types of truncus arteriosus—and Andrew has one of the more complicated types,” Dr. Cook said. “After our initial consultation, Andrew underwent a battery of non-invasive testing—echocardiogram, cardiac CT—to evaluate his complex congenital anatomy. Based on the results of his initial tests, we were concerned about late-onset complications associated with his prior surgical repairs.”
A multi-disciplinary team assembled to examine the case. The team included congenital heart surgeons, cardiologists, a care coordinator and medical social worker, an interventionalist and an electrophysiologist.
“We present the case to the team to discuss and reach a consensus of opinions on treatment,” Dr. Cook said.
Christensen would need a heart catheterization followed by yet another open-heart surgery—one that he hopes is his last, requiring only follow-up procedures after that.
“The good news is that we are seeing more adults with congenital heart disease of great complexity like Andrew’s,” Dr. Cook said. “That means through surgery, interventions and appropriate medical care, more children with heart defects are expected to live well into adulthood.”
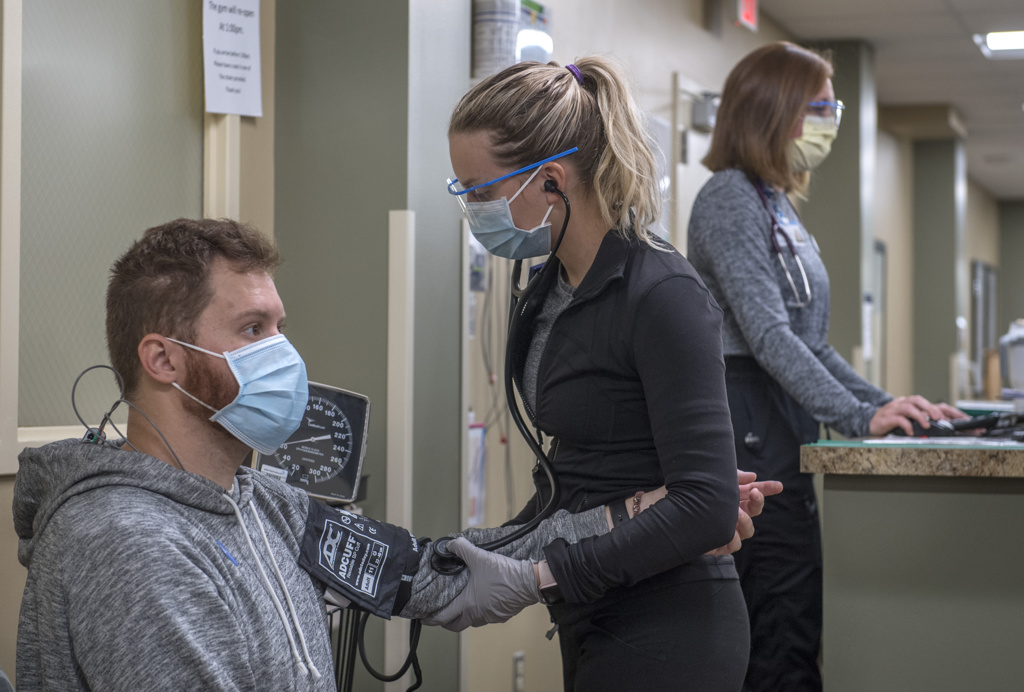
Christensen went to the Meijer Heart Center on July 22 for a cardiac catheterization.
Surgery came the following day.
“We wanted to avoid two separate admissions,” said Marcus Haw, MD, Spectrum Health pediatric cardiovascular surgeon. “We had looked at CT scans of Andrew’s heart. His defibrillator had developed a leak.
“In the CT scan, we saw what looked like an aneurysm,” Dr. Haw added. “A cow’s jugular vein had been used in a previous surgery and the pressure in it had become too high and it can dilate too much.”
Christensen’s past catheterizations and a stent had also narrowed.
Since truncus arteriosus can’t be cured, it’s important that patients undergo lifelong monitoring and regular care to ensure previous surgical improvements align with the body as it grows from child to adult.
“Andrew hadn’t had care in two years,” Dr. Cook said. “Patients with gaps in care are more likely to develop medical problems requiring intervention than those receiving continuous care.”
During a five-hour surgery, Dr. Haw stopped Christensen’s heart with a bypass machine.
“In Andrew’s case, there was a lot of scar tissue surrounding the stents in the pulmonary artery,” Dr. Haw said. “Removing the stents is the best way to ensure that the fibrous tissue doesn’t come back in the future. Once we had rehabilitated the pulmonary arteries, we connected the heart to the lung artery with a new valve and tube graft called a conduit. This may last a long time, but more importantly, it is also suitable for a new valve to be implanted in the tube by a cardiac catheter procedure. This would avoid another open heart surgery for Andrew.
“We are all excited that he is doing so well and look forward to hearing of his progress over the next years.”
New hope
“I was nervous going into it,” Christensen admitted. “I feel good now, still sore, but good. I went in on a Wednesday and I was home by Sunday.”
Gradually, Christensen started walking longer and longer distances.
He felt grateful, he said, for wonderful nurses who cared for him and helped alleviate his anxiety.
“I was more anxious about everything now than when I was younger,” he said. “I understand more now of what’s going on. I talked to a therapist before this, too, and that helped.”
“It is not uncommon that many of our adult congenital patients report symptoms of anxiety prior to upcoming surgeries, especially someone like Andrew returning for a fifth-time re-do,” Dr. Cook said. “Undiagnosed anxiety and depression is present in 30% of adults with heart defects.”
Christensen learned coping skills and realizes how important it is that he not skip a year of follow-up visits with specialists who understand the complexities of congenital heart conditions. He also came away from his recent surgery with a renewed focus on helping others.
“While I was in the hospital, I noticed someone across the hall in another room,” Christensen said. “He was all alone. No one ever came to visit him. It kind of broke my heart. It has me thinking, now that I have this new chance, what I can do for others.”















 /a>
/a>
 /a>
/a>
 /a>
/a>
Andrew,
Thank you for sharing your amazing story. I was also born with Truncus Arteriosus and now have an ICD. I am 38 years old and have had 3 open hearts, my most recent was last year.
I currently work for an organization called Conquering CHD as the ACHD Coordinator, we provide education, advocacy, support and more for patients and families across the lifespan.
The world could use more inspiring stories and adult voices like yours! If you’re interested in learning more about what we do please consider checking out conqueringchd.org or emailing me at jweiner@conqueringchd.org
Thanks again for sharing!
-Jenny