She first began to notice the symptoms more than a decade ago, as a high schooler.
Irregular periods, acne, hair growth.
And yet, a doctor didn’t officially diagnose Ashley Kimble with polycystic ovary syndrome until two years ago, when she tried to become pregnant.
Unfortunately, even though it’s a common disorder and a leading cause of infertility in women, delayed diagnosis is not unusual in such cases.
Polycystic ovary syndrome can often go undiagnosed for months, or years.
“I wish people would have asked more questions and put more thought into what was going on,” said Kimble, now 29. “Just because I am not a typical (polycystic ovary syndrome) patient doesn’t mean I don’t have it.
“It has been a long journey,” she said.
Irregularities
James Young, MD, a reproductive endocrinologist at The Fertility Center in Grand Rapids, said polycystic ovary syndrome may go undiagnosed for several reasons:
- It’s a clinical diagnosis—there’s no particular lab test to verify a patient has it.
- The symptoms vary from woman to woman and they’re similar to those of many other health issues women face.
- There’s no great consensus among doctors about what symptoms a patient must have to reach a diagnosis. Some women may display all the classic symptoms, but others may have only a few.
The typical symptoms of this syndrome, according to Dr. Young:
- Irregular periods, or none at all.
- Infertility. The syndrome disrupts ovulation.
- Increased facial and body hair growth, a result of androgen overproduction.
- Excessive acne.
- Unusual weight gain, despite diet and exercise. The syndrome causes insulin resistance.
- Metabolic syndrome, including high cholesterol and pre-diabetes in severe cases.
As a teenager, Kimble recognized several of these symptoms in herself. She had irregular and extremely painful periods, sudden and severe acne, as well as some excessive hair growth.
Doctors put her on birth control pills to control the symptoms, but her periods remained irregular for years.
“Nobody ever told me to be concerned about it,” she said.
Not until she and her husband, Jordan, tried to become pregnant a few years ago did she begin to wonder. After stopping her birth control pills, she still didn’t get a period for several months.
“I started doing research on my own,” she said. “From my symptoms it seemed like maybe I had (polycystic ovary syndrome).”
Doctors didn’t agree, however, and one doctor suggested her skinny frame would preclude her from developing this syndrome.
Finally, in August 2014, an ultrasound showed many small follicles or cysts around her ovary, confirming polycystic ovary syndrome. However, tests also indicated she did not have the insulin resistance that’s common to many patients with this disorder.
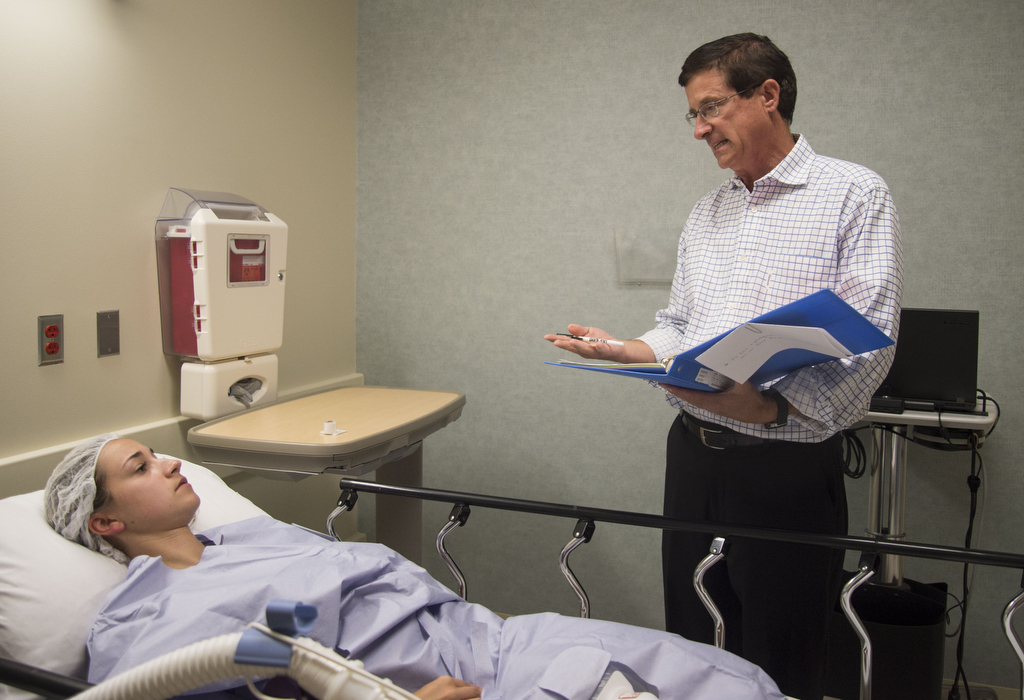
Soon after the diagnosis, the Kimbles went to The Fertility Center for help.
Talk about it
Dr. Young urges patients to provide all the information they can about their symptoms, without embarrassment.
Every piece of information is important.
“As physicians, we need to know everything that’s going on,” the doctor said.
It’s critical to arrive at the right diagnosis and choose the right treatment, regardless of whether a patient is trying to get pregnant, he said.
If a patient is not having periods, she is not shedding the uterine lining. This can lead to other problems, he said.
Polycystic ovary syndrome has been linked to an increased risk of developing several medical problems, including insulin resistance, Type 2 diabetes, high cholesterol, high blood pressure and heart disease.
There are treatment options, Dr. Young said, including:
- Birth control pills to regulate periods.
- Medications to promote ovulation.
- Medications to decrease androgen production.
- Electrolysis or laser hair removal.
“If you have (polycystic ovary syndrome), there is something physically wrong and we have ways to treat that,” Dr. Young said.
Kimble said it’s been a long journey of ups and downs, but she has learned much and she’s willing to share her experiences.
“I’m always willing to talk about it,” she said.
She encourages other young women to keep asking questions until they get the answers they need.
“You really need to advocate for yourself with your doctor or OB,” she said. “I don’t want people to be afraid to speak up. The clock is ticking, and I don’t want people to miss out on any opportunities.”

















 /a>
/a>
 /a>
/a>
 /a>
/a>