As patients battle the life-threatening effects of COVID-19, they have a powerful ally in their corner.
Not a single person. Or medication. Or new treatment.
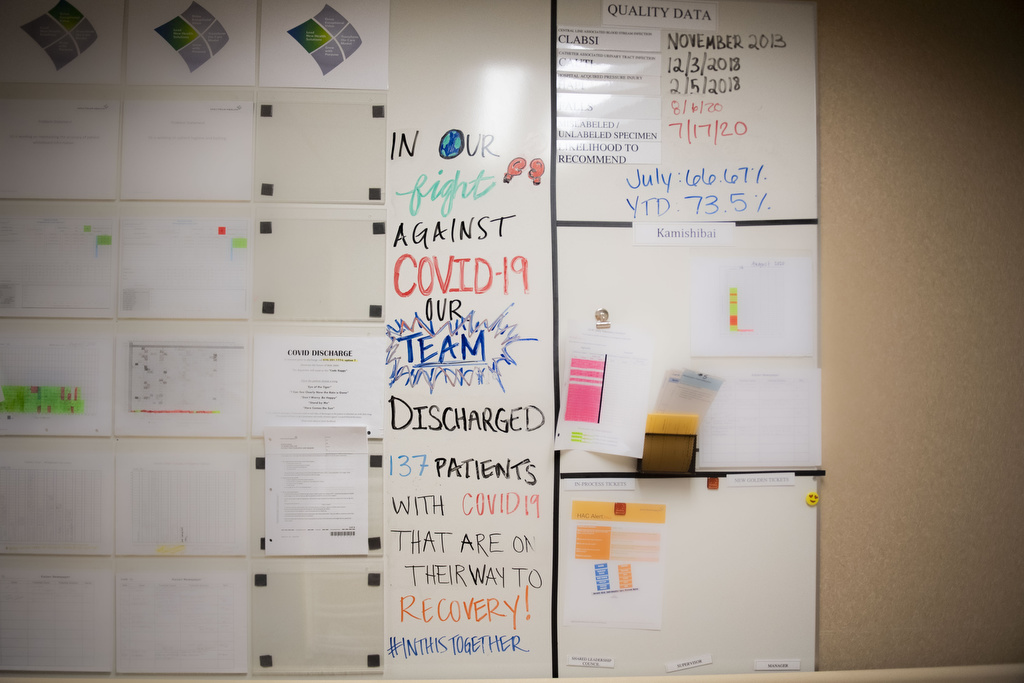
They have a team—a dedicated group of health care professionals ready to work together to treat patients who have COVID-19.
A sense of teamwork, forged through experience caring for other seriously ill patients, has been invaluable as front-line health care workers face the unknowns that come with the new coronavirus.
That has been apparent from the first days of the pandemic on the progressive care unit at Spectrum Health Blodgett Hospital. The unit, staffed by nurses with specialized training in respiratory interventions, provides a level of care that is between the intensive care unit and a medical-surgical unit.
At times, patients with COVID-19 occupied every bed in the 22-bed unit. Although the number of hospitalized COVID-19 patients has declined, the team stands ready to meet a surge in demand, if needed.
“They are absolutely ready to do it again if they are called upon,” said Audra Nelson-Arnett, nurse manager for the unit. “They step up to the plate when needed.”
That team encompasses nurses, physicians, pharmacists, nutritional and environmental services specialists, as well as physical, respiratory and occupational therapists.
“We always knew we were a strong team and knew what we were doing, but this (reinforced) how strong we are as a team,” Holly Drew, RN, said.
When the first patients arrived in the hospital, team members set aside their own fears to respond with calm efficiency to the needs of their patients.
“They stepped up, were resilient and put on a brave face and they took care of these patients,” Nelson-Arnett said.
“It was just amazing to me. They just took it in stride. They asked good questions. And they provided excellent care to these patients.”
That dedication continues, as team members back each other up and apply all they have learned about this virus in the past six months to help those affected today.
Meet some of the members of the team:
Holly Drew, RN
As Drew shopped at a grocery store one day, a woman approached and said, “I know you. You look so familiar.”
In a flash, she realized why.
“You were my nurse when I had COVID,” she said.
She turned to her husband and said, “This was my favorite nurse. She just sat there and laughed with me and made me feel so much better.”
Drew marveled. In caring for patients, she wears a face mask, face shield, gown and gloves. Only her eyes are visible.
And yet the woman recognized her—and clearly appreciated her care.
“It did make me feel really good,” Drew said. “It is why I do what I do. And it is why I continue to do what I do.”
The encounter highlights the way nurses go out of their way to show compassion and kindness to patients who are separated from their loved ones as they battle COVID-19.
“COVID is scary. When you come in here and are told you have COVID-19, you’re scared,” she said. “You are scared you are not going to survive.
“We are their sounding boards. We are the ones sitting in the rooms with them, walking them through these processes.”
Ben Busman, DO
Dr. Busman treated some of the first patients with COVID-19 at Blodgett Hospital.
“Those early days were trying, to say the least,” he said.
But in the past few months, the medical team has learned much about the disease.
“We are having increasingly better outcomes for our patients as we recognize how to treat this illness—what works, what doesn’t work, what to watch out for,” said Dr. Busman, a hospitalist and section chief.
“This illness is still a scary thing, but it feels much different than it did four months ago. We are much better equipped to deal with this illness.”
He admires the way the medical team responded in the early days of the pandemic, despite the unknowns.
“I didn’t pick up on a lot of trepidation and anxiety from the staff,” he said. “They were here to care for patients, and they did an excellent job.
“In a way, it has unified us like nothing ever has. There’s a lot of good to learn from that and to carry those lessons forward.”
Dr. Busman urges continued vigilance to prevent another surge in cases.
“We are holding our breath, hoping everyone will do what they can to mitigate the spread of this illness,” he said. “We have seen how quickly things get bad.”
He hopes the general public will embrace the use of face masks—to keep others safe from illness.
“It’s to keep someone’s fragile loved one from dying,” he said. “And I think we can all recognize the importance of that.”
Allie Van Laar, RN
“We’ve seen a lot of loneliness from patients, just not having the visitors they would normally have,” Van Laar said.
Nurses bring iPads into the patients’ rooms so they can communicate with loved ones. But only their medical caregivers provide the face-to-face emotional support.
She recalled one unique situation, in which a woman was able to visit her husband.
The couple, in their 90s, both were hospitalized with the virus. The woman’s condition improved. Before she went home, the nurses brought her to her husband’s hospital room.
“They embraced, and the husband seemed to do a lot better knowing his wife was in the room with him,” Van Laar said.
Tears flowed—from the patients, nurses and family members watching through an iPad.
“The husband passed away the next day,” Van Laar said. “Thankfully, (his wife) got to see him and talk to him and love on him a little bit.”
Van Laar also recalls the joy of patients who recover and head home. In the early days, the team played a victory song and lined the hall, clapping as the patient rolled by in a wheelchair.
One woman videotaped the team as she left.
“She just was wheeling down the hallway, filming us and sobbing, so grateful to make it out of here after a long hospital stay,” Van Laar said. “I think that made all of us, as a team, feel pretty good about the work we are doing here.”
Sarah Carlson, PT
“I remember my first patient that I saw with COVID-19 and just how sick he was,” Carlson said. “I’ve never worked with a patient whose (blood oxygen level) went down so low so fast.”
As a physical therapist, she begins working with patients as soon as possible, even those still in the ICU.
“We are getting them sitting up, even on a ventilator,” she said. “Most of them don’t even remember that we were there.”
She continues physical therapy sessions with patients when they move to the progressive care unit. When they become discouraged as they try to build back physical strength, Carlson gently reminds them of how far they have come.
“It’s nice when they are progressing and you are able to give them that encouragement,” she said.
As the mother of two young children, Carlson worried at first about bringing the virus home with her. With protective equipment and safety measures in place, however, she feels confident she and her family can remain healthy.
Now her kids are excited about going back to school, and she urges them and others to wear masks and practice social distancing—so school and other activities can continue.
“These kids need normalcy in their life again,” she said.
Andrew Kuiper, RN
Kuiper understands that it might be difficult for people to grasp the seriousness of COVID-19 if they do not work with patients or have a loved one who is ill.
“But when you are a few feet away from someone that can’t breathe—I don’t know how to put into words what that’s like.
“It’s very serious.”
Of all the patients he has seen, those with COVID-19 are the most afraid.
“As nurses, that’s where we can really come in to help them, to calm their fears a little bit and tell them what to expect and try to get them through it,” he said.
As patients learn about the treatments available, including convalescent plasma and antiviral treatments, it helps ease their minds.
According to the unit’s unofficial tally, more than 150 patients have been able to go home or to a rehabilitation facility.
Each milestone on the way to full health represents a victory.
“Those days when they are hanging steady, getting a little bit worse—and finally turn the corner and they’re starting to feel better, there is no better feeling,” Kuiper said.



















 /a>
/a>
 /a>
/a>
 /a>
/a>