Melissa Fessenden relishes the private, cozy experience of a home birth.
She delivered her first five children in the comfort of her home, guided by a trusted nurse midwife, tended with loving care by her husband, Shawn.
But, oh, how different it was with baby No. 6.
All the latest technologies and techniques, a host of medical specialists gowned and gloved, a bright operating room filled with beeping monitors—all the king’s horses and all the king’s men—came together to usher Willow Emma Grace Fessenden safely into the world.
So different, this birth. But every bit as blessed and meaningful for her grateful mom and dad.
“It was a different kind of beautiful,” Melissa said. “It was a completely different experience and yet still full of beauty.”
Because a large tumor blocked Willow’s airway, the physicians performed an EXIT procedure in which just the baby’s head is delivered, giving doctors time to treat medical issues before the child is born.
It was just the third time Spectrum Health physicians have performed this highly specialized and carefully orchestrated cesarean section.
Busy and adorable
The Fessendens learned of Willow’s unique needs at her 20-week ultrasound.
As she underwent the routine screening, Melissa watched the monitor, captivated by the baby’s antics.
“Willow was so active during it, so busy being adorable,” Melissa said. “She was grabbing her nose and ears and you could see her tongue moving.”
She and Shawn looked forward to the day they would welcome her to their home in West Michigan, about an hour north of Grand Rapids. In a house lovingly remodeled by Shawn, surrounded by trees and a short walk from the river, they live with their children, Ellia, 9, Lyla, 7, Elowen, 6, Oliver, 3, and Lydia, 1 1/2.
After the ultrasound, Shawn cautiously told his wife he noticed something unusual about the baby’s neck. Examining the photos at home, Melissa was surprised she had not noticed the lump just under the right side of her chin.
A quick call to their nurse midwife and soon they had an appointment with the maternal fetal medicine program at Spectrum Health.
“I always said I would go to a hospital if I needed to,” Melissa said. “I prefer a home birth, but we want what’s safest for Willow.”
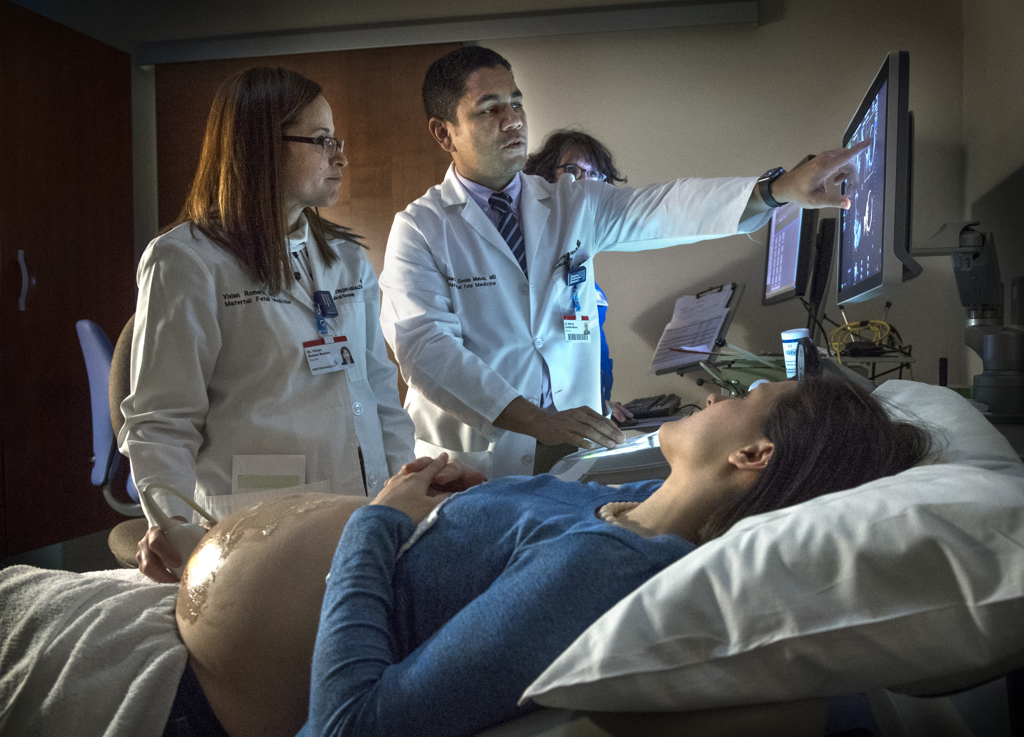
Marcos Cordoba Munoz, MD, a maternal fetal medicine specialist, performed another, more detailed ultrasound.
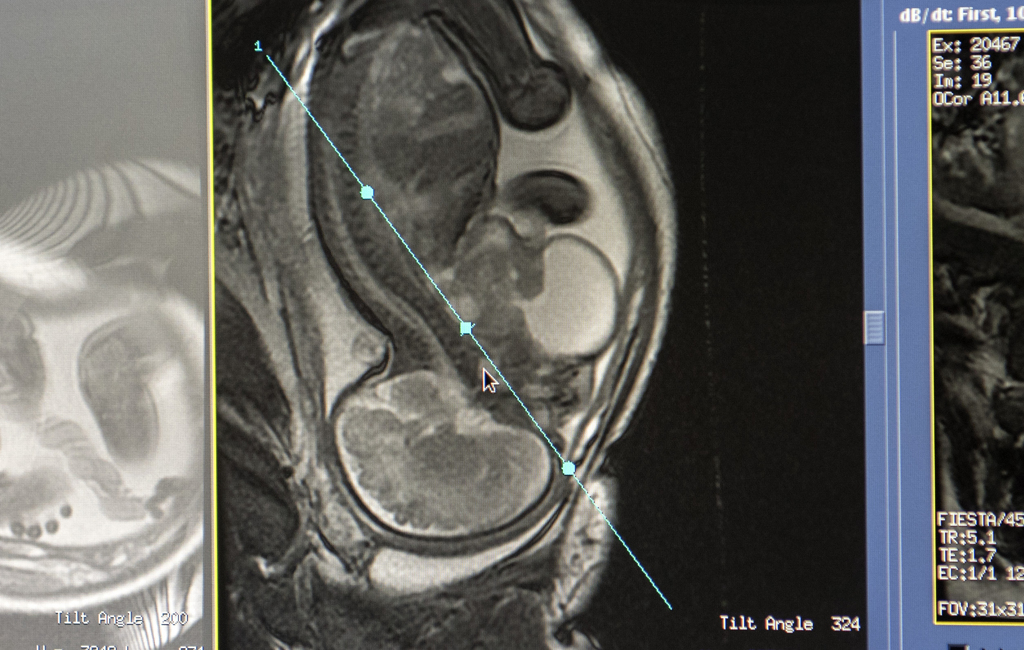
It revealed that the baby had a cervical teratoma, a tumor that arises from immature cells in the neck. The condition occurs in 1 in 20,000 to 40,000 live births.
The tumor, a combination of solid and cystic components, measured about an inch across when discovered at 20 weeks. By 31 weeks, it had grown to 3 inches.
Though most are benign, the tumor can block the baby’s airway. A newborn’s first moments can become a life-and-death struggle to breathe.
“We probably wouldn’t have a baby who was alive if we didn’t know about it ahead of time,” said Chad Afman, MD, a pediatric otolaryngologist. “It would have been a very scary and difficult surprise to deal with if that was unrecognized until the very moment of delivery.”
I thought I would be nervous and anxious. But God gave us such peace.
Early detection, however, gave the maternal fetal medical specialists time to prepare for the EXIT procedure, or ex-utero intrapartum treatment. As they monitored the health of mom and baby, they began to work with a team of adult and pediatric specialists to plan for Willow’s delivery.
With help from Spectrum Health Innovations and the Congenital Heart Center of Spectrum Health Helen DeVos Children’s Hospital, they printed a 3D model of Willow’s head and neck. The white plastic model, small enough to fit in the palm of a hand, showed the peaceful features of Willow’s face and the teratoma that swelled on her neck. The doctors used the model to explain to the Fessendens the risks Willow faced and their plan to address them.
Melissa and Shawn met with each anesthesiologist, surgeon and physician who would be involved in the delivery and Melissa’s care.
“They’ve been amazing,” Melissa said. “We were able to ask all of our questions. We definitely appreciated their transparency and thoroughness.”
As they waited for Willow’s arrival, they drew on their faith to cope with their fears.
“I feel like the Lord is saying, ‘I made your body to breathe for her now,’” Melissa said. “The doctors will be there for her when it’s time to breathe.”
The team approach
The EXIT procedure occurred 37 weeks into Melissa’s pregnancy. Early on that November morning, two dozen doctors, nurses, respiratory therapists and technicians gathered in a hallway near the operating rooms at Spectrum Health Helen DeVos Children’s Hospital.
“We have two patients and we have two teams here,” said Vivian Romero, MD, a maternal fetal medicine specialist, as she led a discussion about each person’s role in each step of the delivery.
After Melissa was wheeled into the operating room, Dr. Romero and Dr. Cordoba began the C-section.
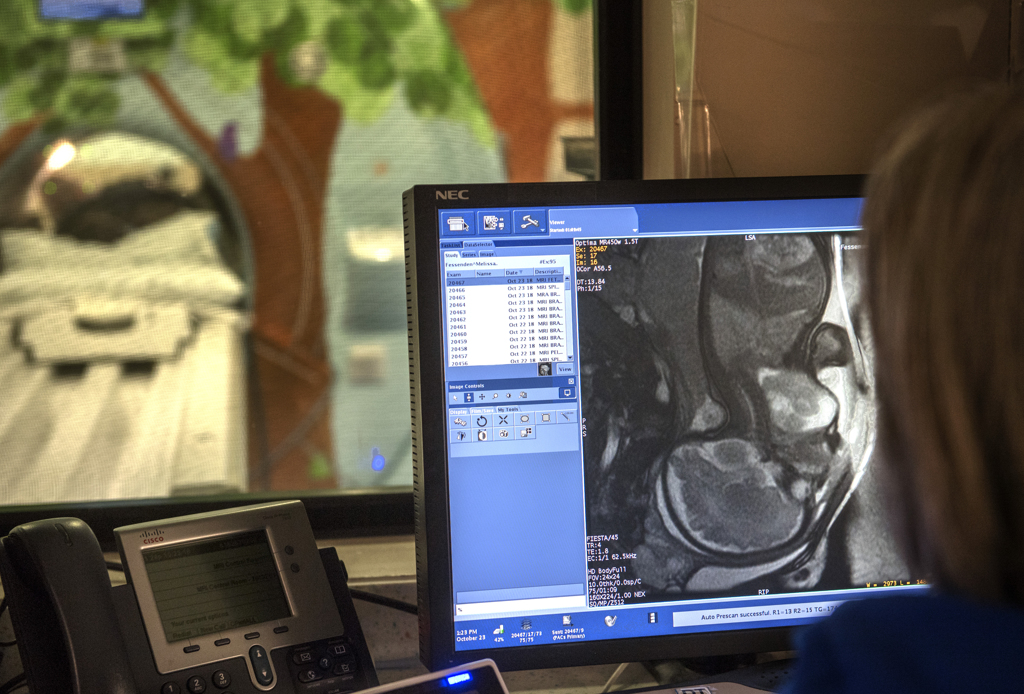
They made an incision in the abdominal cavity, but did not open the uterus. They placed a needle in the tumor, using ultrasound guidance, and drained 8 ounces of fluid from the cyst. Reducing the size of the cyst would make it possible to deliver Willow through a small uterine incision.
Because mothers face an increased risk of excessive bleeding during an EXIT procedure, they used a special stapler in opening the uterus.
“It will cut but at the same time clamp the edges of the uterine incision to prevent bleeding from the edges while we are delivering the baby,” Dr. Cordoba said.
As the amniotic fluid rushes out, the uterus normally begins contracting. But here it remained relaxed, thanks partly to medication from anesthesiologist Eric Egeler, MD, and partly to catheters replacing the fluid and keeping the uterus full.
The doctors eased Willow’s head and shoulders out. She did not draw breath. She didn’t need to. Still nourished by her mother, she lay between womb and world, almost born—but not quite yet.
Immediately, an ultrasound monitor was placed on her chest, providing the team with images of her steadily beating heart.
The surgeons made room for John Huntington, MD, a pediatric anesthesiologist, to intubate Willow. Using a video camera-equipped scope, he examined the airway as he placed the breathing tube between her vocal cords.
Having the fluid drained from the tumor improved the exposure of the airway, he said.
“It took a minute or two to get a breathing tube in place,” he said. “It seemed to go fairly easily.”
Although relieved it went well, he had assistance available just in case. Pediatric surgeon Emily Durkin, MD, and Dr. Afman were prepared to perform surgery if needed.
Dr. Huntington held Willow’s head and breathing tube, using a resuscitation bag to keep air flowing to her lungs, as Dr. Cordoba and Dr. Romero brought Willow completely into the world. They clamped the cord, breaking the connection to the placenta. At that moment, Willow officially was born—a beautiful, pink-cheeked, 6-pound, 15-ounce baby girl with a full head of brown hair.
Dr. Huntington and Dr. Afman gently carried Willow and the breathing tube to the warm incubator, where neonatologist Mitchell DeJonge, MD, and a team of nurses from the neonatal intensive care unit took charge of her care.
Meanwhile, the maternal fetal medicine specialists finished the C-section. Melissa fared well, losing little blood.
In all, more than 30 medical professionals participated in the delivery.
“I liked how we all worked together,” Dr. Huntington said. “There were a lot of good people in the room. You always want to have more backup plans than you need.”
Gratitude
As Willow slept in her incubator, a ventilator delivering oxygen to her lungs, nurses wheeled her mother’s bed from the recovery room to the Gerber Foundation Neonatal Center at Helen DeVos Children’s Hospital.
Raised to a seated position, Melissa reached out and stroked her daughter’s forehead. Willow’s eyes opened and closed briefly. She shook, silently crying, tears gathered in the corner of her eyes.
“It’s OK,” Melissa said. “Mama’s here. You’re OK.”
But Willow’s safe arrival had been just the first hurdle the newborn faced.
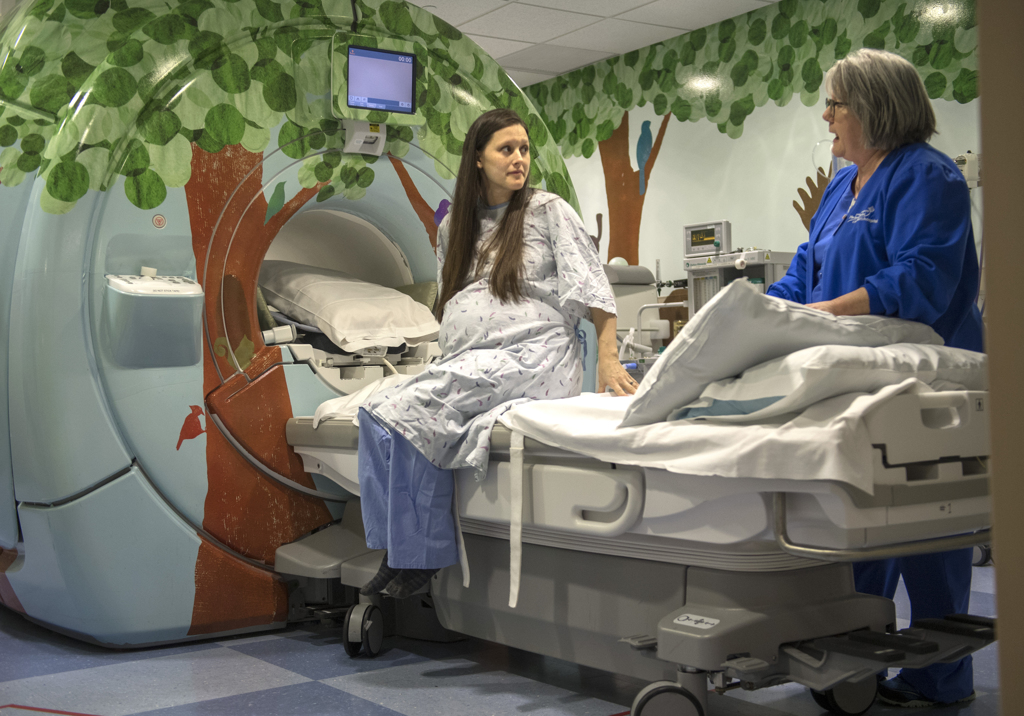
Next would come surgery to remove the cervical teratoma, which doctors scheduled to take place four days after delivery. They first wanted to make sure Willow had become stable. She had an MRI, which gave doctors a clearer picture of what they would encounter during surgery and showed Willow had no heart defect.
On Thanksgiving, the day before the operation, Melissa sat beside Willow’s crib. She felt torn—she wanted to remain thankful for her blessings, but she still wished her daughter could be free of tubes and wires. She ached to just reach into the crib, pick up her baby girl and hold her close.
Jason Yakes, RN, Willow’s nurse, administered medication, describing a dose as a “bolus” to help her through the coming surgery.
And then Melissa got her wish. With help from a respiratory therapist, Yakes carefully lifted Willow from her crib and placed her in Melissa’s arms.
She cradled her daughter for more than two hours, her heart swelling with gratitude and peace.
“After being told for the last three months that I would likely not be able to hold Willow ’til after her surgery, this felt like a small miracle. I felt like I got a bolus of love to push me through tomorrow,” she said.
Surgery
Early the next morning, Melissa and Shawn gave Willow a kiss and watched as she left for surgery.
Dr. Afman and Dr. Durkin performed the complex, delicate operation to remove the cervical teratoma. Dr. Huntington, the physician who intubated Willow after birth, provided the anesthesia for the operation.
As expected, fluid had re-accumulated in the cyst, which now measured 5 inches across.
“Normally, with a surgery like this, we use a special breathing tube that monitors the functions of the nerves that control her vocal cords,” Dr. Durkin said. “But they don’t make the tube small enough for a baby her size.”
Dr. Afman came up with an alternative—using micro needles and electrodes—to help them monitor and protect the vocal cord nerves during the five-hour operation.
It was a benign teratoma. It was 100 percent removed. Her prognosis is excellent.
The surgeons found the tumor had started in the thyroid gland, which was completely replaced with tumor. Although Willow may not have a functioning thyroid left, she can take a thyroid hormone replacement, Dr. Afman said.
Just due to its massive size, the tumor had additional effects on the surrounding structures. The airway was distorted, and the carotid artery was displaced far out of its normal position.
The right internal jugular vein, which carries blood from the head to the heart, was not present.
“It was either obstructed by the mass or never developed,” Dr. Afman said. He added that Willow can function with just the left jugular vein.
The right recurrent laryngeal nerve—the nerve to the vocal cord—could not be found in its normal position during surgery. And initially, Willow had no true vocal cord function on the right side. But in the coming weeks, that changed.
“We noticed that Willow’s voice was becoming stronger over time and her breathing and swallowing were improving,” Dr. Afman said. “On Christmas Eve, I was able to take another look at her vocal cord function and report the happy news to family that both vocal cords are now working normally.
“I expect her to have no trouble with eating, talking, or breathing.”
The pathology report on the tumor showed good news.
“It was a benign teratoma,” Dr. Durkin said. “It was 100 percent removed.”
While doctors will continue to monitor Willow, Dr. Durkin said, “her prognosis is excellent.”
Willow the hero
For Willow to survive and thrive through her medical challenges, it took highly specialized, carefully coordinated care, Dr. Durkin said.
“This type of treatment really depends on everyone being at the top of their game for their individual job,” she said. “I needed everyone in that room in order to do my job, and they did, too.”
The best outcome for Willow began with the loving dedication of Melissa and Shawn.
“Despite the fact that this was such a departure from everything this family had experienced in the past, they were willing to listen and participate and understand,” Dr. Durkin said. “They just wanted the best outcome for their daughter.
“There really is no hero in this story—other than Willow and her family.”
For Melissa, the experience proved far more personal than she expected.
“From the beginning, I felt listened to and respected,” she said. “I didn’t imagine it would be such a positive experience for being as intense as it was.”
She had been surprised at how calm she felt when the time came for Willow’s birth. She entered the operating room filled with bright lights, monitors and a host of medical professionals.
“I thought I would be nervous and anxious,” she said. “But God gave us such peace. I just thought, ‘She’s going to be here soon.’”
Hope for the future
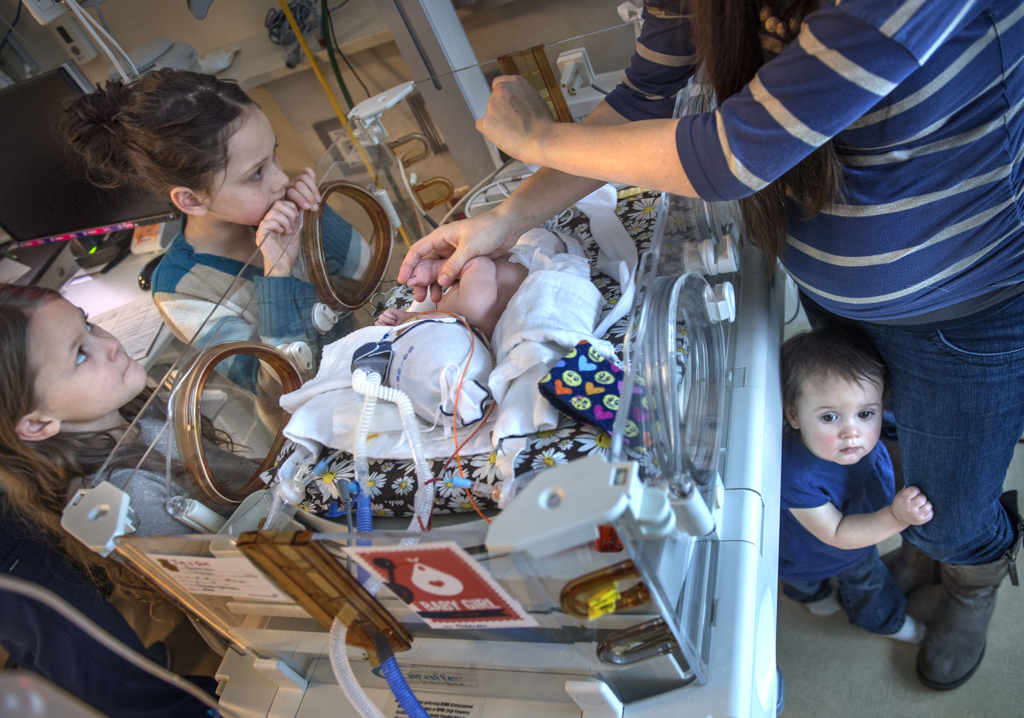
Melissa lifted Willow from the crib, carefully working around her feeding tube and the cords attached to the heart rate and respiratory monitors. She sat in the armchair as her other children clustered around.
Willow’s right eye fluttered open, then the left.
“Look at you!” Melissa said.
Three-year-old Oliver placed a toy stethoscope on his baby sister’s chest.
“I’m going to heartbeat her,” he said.
At 3 weeks, Willow no longer needed breathing support. The incision from her surgery, tucked under her chin, had healed. She had already begun to grow. She would soon undergo a swallow test to check her readiness to eat without aspirating milk into her lungs.
Melissa looked with optimism toward each milestone, especially the day Willow could go home.
“I can just imagine her swinging in the backyard with the kids,” she said. “I know she will always carry some signs from this journey. But I hope she will see how God has used this whole situation to really bring something beautiful from it.
“I feel God’s peace. A supernatural peace beyond understanding.”



































































 /a>
/a>
 /a>
/a>
 /a>
/a>
What a beautiful story of God’s great mercy and grace using the skills and compassion of the professional world to give an amazing outcome. What an encouraging read!
This is such a beautiful story, it brought tears as I read it! Wonderful team of doctors! A beautiful family and new baby!
A beautiful family, indeed. We really enjoyed getting to know Melissa, Shawn, Willow and her big sisters and brother.
What a miracle!
What a wonderful story! Once again, I am thankful for our top notch West Michigan medical community. What impresses me the most is that these experts in their fields are also caring team players who continue to make their patient (and family) the center of their care and procedures. Spectrum Health has figured out how to hire fine human beings!
The Fessendens and their doctors, nurses and caregivers truly made a great team.
Grand Rapids is blessed having such a great medical team
What a beautiful family. The story was beautiful as well, telling the families journey. Willow is a beautiful little girl. So thankful for the medical team that took care of this precious family. My granddaughter, Emma Grace is now 3. She went thru the exact procedures. She had a multi cystic teratoma on her tongue. She is a now healthy toddler. Has some issues with her tongue, but she functions pretty normal. God bless hour beautiful family.
So interesting that they share a name and such a rare condition! Our daughter needs thyroid medication but otherwise is expected to live a normal, healthy life now that her second vocal cord is working! I pray your granddaughter continues to do well! Thank you for sharing!
The whole team there at Devos is phenomenal! Thank you Sue Thoms for portraying our story so beautifully! We praise God for everything He has brought us through and continues to bring us through. We know He is good, always, no matter what, but we are so grateful that we are able to raise our baby girl! We are truly blessed!
Chris Clark and I really enjoyed getting to know you and your family, Melissa. Thank you so much for sharing your story. It was an honor to write it.
Chris Clark did an amazing job telling our story through his photos. Thank you Chris! It wouldn’t be the same without you!
Dr. Chad Afman is my nephew – SO proud of him!!! And he is so humble – just makes him extra special!
What a beautiful and loving family and story! I am so thankful to hear a family give God praise! And little Willow is so incredibly blessed to such a wonderful family to go home to! Thank you to everyone involved. God has an extra close eye on you all. Many, many blessings to you!
I am so thankful to have read this beautiful story…amazing!!! Thank you to all who took part. And praise God for not only creating such a special little girl but also blessing her caregivers with skilled hands and her parents with strong faith.
Thank you for your lovely words of encouragement and blessings, Mary! And thanks for being a Health Beat reader. We appreciate you!
What a fascinating story! It’s so wonderful how technology prepared the medical staff to know Willow’s issue before she was even born and allowed them to be prepared