In the fall of 2018, fourth-grader Naomi Gomez sat at a desk in Harbor Springs, Michigan, learning spelling, writing, multiplication and division.
What she never learned, and never wanted to, was how to live with cancer.
“It started in October, November of 2018,” said Naomi’s mom, Jessica Creary. “She complained of her ankles hurting, her knees hurting and being really tired. She was losing her appetite, but we thought maybe that was just a phase, that things weren’t tasting good to her.”
But Naomi’s weight kept dropping.
“We kept going back and forth to the pediatrician,” Jessica said. “They thought it was growing pains. But between November and December, Naomi dropped about 11 pounds. She was only 93 pounds to begin with.”
That’s more than a 10% drop, in a month, for a 9-year-old.
“Naomi has always been a really good eater,” Jessica said. “She’s never been heavy or overweight, just always a really healthy size, but the weight loss was pretty drastic.”
As with any person we see daily, the weight loss didn’t jump out to Jessica. When she looked at photos over those months, though, the trend revealed itself.
“It was so gradual,” she said. “At her age, she’s just starting to discover her independence and is starting to do things on her own. We thought maybe her aches and pains were her way to try to get out of school. Kids have been doing that since the beginning of time. I know I did.”
But as December snow fell, and Christmas neared, more symptoms surfaced.
“She started falling asleep in school,” Jessica said.
A former pediatrician-turned-school-counselor alerted the family.
“One teacher told me she was snoring,” Jessica said. “She wasn’t sleeping well at night. I didn’t know this at the time, but a couple of times I guess she woke up and went into my mom’s room because she wasn’t feeling well. My mom lives with us. My mom is an oncology nurse.”
Grandma suspected something was up with Naomi, but it seemed far-fetched. Impossible, really.
“My mom being a nurse went to the worst-case scenario, ‘What if she has cancer?’” Jessica said. “I said, ‘Mom, that’s because you’re a nurse. There’s no way.’ I had a completely different picture in my mind.”
Jessica set up family counseling sessions, thinking Naomi’s weight loss and lethargy may be pinned to something going on at school, or perhaps bullying.
‘My insides are shaking’
“One morning, I woke her up for school and she was crying,” Jessica said. “She said, ‘Mom, I feel like my insides are shaking.’ She related it to feeling like her bones were vibrating. I said, “If you’re not going to school, we’re going to the pediatrician.’”
The Northern Michigan pediatrician didn’t see anything amiss. But blood tests proved differently.
Just hours after the blood draw, the pediatrician called and told Jessica they sent the blood test results to the pediatric hematology and oncology clinic at Spectrum Health Helen DeVos Children’s Hospital.
Soon, the pediatrician called to tell her the hematology and oncology clinic wanted to see them the next day at 8 a.m.
“I was at a daycare looking at putting our son in a new daycare,” Jessica recalled. “I started crying. I called my husband (O.J. Creary). We drove down that night and stayed at the Renucci House. That night and the next morning are kind of a blur to me.”
Jessica expected a simple diagnosis.
“I thought maybe it was anemia or something else,” she said. “From the moment we got there, it was like they knew, but couldn’t tell us because it hadn’t been confirmed.”
The “blur” became a blinding reality, a nightmare no parent wants to live through. Following bone marrow tests, on Jan. 16, doctors diagnosed Naomi with B-cell acute lymphoblastic leukemia. The news shattered Jessica and O.J.
“I wasn’t expecting a cancer diagnosis,” Jessica said. “Before this, I had never had an encounter with someone who had fought through cancer. I never would have guessed.”
Social workers visited the family. Jessica left the room. And cried.
“The diagnosis was scary,” Jessica said. “But doctors were really great at putting things in layperson’s terms and making it easy to understand what was going on and what we would need to do to treat her.”
‘I didn’t really know what cancer was’
Naomi handled the news with courage and grace.
“My first reaction was, ‘Huh?'” Naomi said. “I didn’t really know what cancer was. I thought that meant I was going to die.”
Naomi remained strong.
“Still to this day, she’s never had a breakdown moment,” Jessica said. “She’s never looked at me and asked, ‘Why me?’ She’s super strong, like ‘that’s life, and life is moving on.'”
Hospital staff helped make Naomi as comfortable as possible.
“One of the nurses we had, Stephanie, she went way over and beyond what I have ever seen a nurse do,” Jessica said. “She sat with Naomi on her bed. She talked to her not like a sick child, but talked to her like a kid she was hanging out with. She said, ‘We’re going to be new buddies.’ It was a sigh of relief.”
Naomi spent 10 days in the hospital, receiving IV chemotherapy, with her mom and dad beside her.
She then received a longer-acting chemo that stays in the system about 10 days.
The family returned home on Jan. 25.
“They send you home feeling like, ‘OK, we got this, we’re going to follow this treatment and conquer this. Cancer who? We’re going to beat this.’ You don’t feel like this is something that’s going to be the end of her. They instilled nothing but hope, like no matter what happens, they’ve got our back through it all. We came home on a positive note.”
But the positive note soon turned to chaotic discord.
Surviving a stroke
Headaches, “pounding pain, like a hammer,” Naomi described.
At first, the family thought it may be residual chemotherapy effects. Then, she started vomiting.
“She’s complaining of this piercing headache,” Jessica said. “She’s on the sofa, grabbing her head. I took her to the emergency room in Charlevoix. It’s a blessing we did because Charlevoix is maybe two blocks from the airport.”
Blizzards and winter storms moved across the state, causing treacherous driving.
“We got her to the ER and she started having seizures,” Jessica said. “She was groaning and just staring. They rushed her in for a CT scan and that’s when we found out she had had a stroke.”
Doctors induced a coma, intubated her and in the most tense moments imaginable, attempted to take Naomi by Aero Med Spectrum Health to Helen DeVos Children’s Hospital.
“They were on the phone with ICU at DeVos,” Jessica said. “They couldn’t do the helicopter because of the weather so they did a small jet. The weather kept getting worse. As soon as we got to Grand Rapids, they decided she needs to be in a deep, deep sleep because she has a severe brain injury.”
A machine monitored Naomi’s brain activity, which had been reduced to little blips.
“They explained they had to do this to let the brain heal,” Jessica said. “They wanted to give her the best chance possible.”
An MRI confirmed a stroke. When a doctor explained what had happened to Naomi, he also shared the possibility she might not survive.
“I just fell to the floor,” Jessica said. “It’s a feeling you can’t describe. There aren’t the right words to describe the sensation that goes through your body when they tell you your child might not make it. It’s very scary, but I decided, no, I’m not going to back down until I know for a fact this is the end of the road.”
Because of the fragility of the situation, pediatric neurosurgeon M. Michael Bercu, MD, contacted Paul Mazaris, MD, a Spectrum Health Medical Group neurosurgeon who typically works on adults.
“He said, ‘We’re only going to try once, because it is a very fragile, delicate situation,” Jessica said. “He did an angio where they go up through your thigh to try to bust through the clot. He said, ‘We’re going to try, but we don’t know if it’s going to work.’”
A rock. A hard place. And there rested Naomi’s fate.
James Fahner, MD, division chief for pediatric hematology and oncology, said Naomi’s chances of survival were slim, but praised the collaboration between pediatric neurosurgery and adult interventional neurosurgery.
“We were not sure if she would live,” Dr. Fahner said.
Plummeting vital signs
“It was a lose-lose situation,” Jessica said. “It’s a pretty humbling experience when you see even the doctors have concern on their faces.”
After a four-hour surgery, finally, some hopeful news.
“He came back and said they got almost 80% of the clot and they were able to bust through to create blood flow,” Jessica said.
But the next day, Feb. 1, hope turned to fright once again. Naomi’s vitals plummeted. Her heart rate dangerously dropped into the 30s. Her blood pressure arced to 240/150 and her body temperature slumped to dangerous levels.
Staff rushed a portable MRI machine into the room. The scans showed a second bleed in the same area of the frontal left lobe.
“They ended up doing a craniotomy and removed about one-quarter of her skull,” Jessica said.
The family lived day-to-day. About a dozen doctors visited every morning. The activity brought comfort, somehow.
“I know it sounds weird, but there was never a moment where I felt alone,” Jessica said. “There was never a moment that I didn’t feel they didn’t care for my child as much as I do. It was pretty amazing.”
One nurse asked about Naomi’s favorite songs. While Jessica and O.J. grabbed something to eat, the nurse loaded a playlist for the young patient and sang to her.
Because of the brain injury, the room lights remained low. Music therapists softly played the guitar and sang. Naomi received CT scans every four hours.
“We had a fantastic medical team, but definitely could not have done it without our faith,” Jessica said. “The doctors, nurses and chaplain team prayed with us.”
On Feb. 6, doctors stopped the coma-inducing medications. Naomi remained in an ICU room until Feb. 15 and left the children’s hospital nine days later.
Difficult days didn’t end there. Doctors predicted she would need three months of therapy to learn to walk, talk and resume normal activities. Naomi rocked it out and finished therapy in three weeks, although her headaches continued. Light bothered her so much she stayed in a dark room with sunglasses on.
“It was a slow process when it came to speech, remembering words and remembering what she’s trying to say,” Jessica said. “There has been some damage done by the stroke. It took some memories from her.”
Naomi gets around with a walker, and maintains her positive attitude. She hopes to someday dance again.
‘I feel alive’
“From the time she could sit up, she has been a mover and a groover,” Jessica said. “She would move around like a ballerina whose been taking classes at Juilliard. Naomi is like an explosion of sunshine and everything that is good-natured in this world.”
In November, Dr. Bercu replaced the skull flap. A few days after Christmas, she underwent another MRI and planned to return to school.
Jessica said she and her family are grateful for the many friends, family members, co-workers and medical personnel who walked through the dark days with them, supporting them with love, light, food and supplies.
“Naomi is doing fantastic,” Jessica said. “She is pretty amazing. Naomi has to just smile at you once and you’re like, ‘Holy cow, this girl’s got it.’ She teaches me how to just rock life. It’s pretty awesome.”
Naomi said she’s feeling great.
“I feel alive, kind of like a ping-pong ball when it bounces across the table,” she said, giggling at her self-made simile.
Naomi has always seemed to be drawn to the medical field and her curiosity helped her endure her hospitalization and treatments.
“I think it was actually intriguing to her,” Jessica said. “She watches everything intently and asks questions—‘What is that for?’ and ‘Why do you do that?’ I think that I was weaker and had more moments of weakness than she has. She has been steady as a rock.”
When asked recently if she’s still interested in the medical field after all she’s been through, Naomi shouted an emphatic “Yes!”
She wants to become a medical examiner.
“I want to find out how people died,” Naomi said enthusiastically. “You know, solving crimes.”
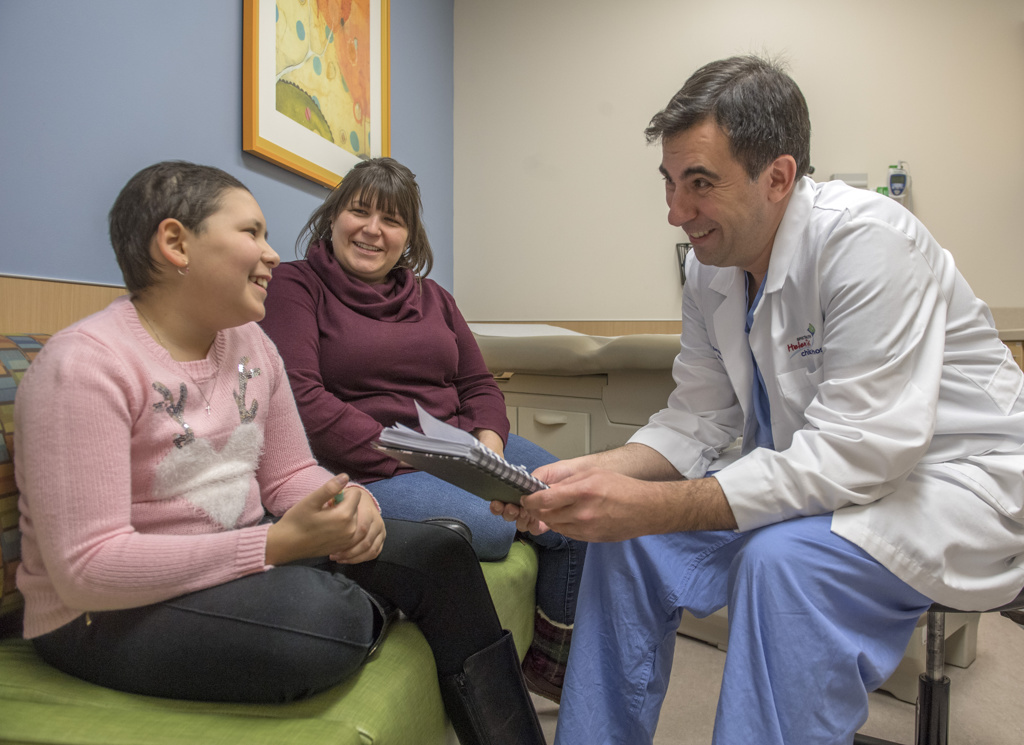
Dr. Fahner said he’s impressed with Naomi’s outcome.
“She has worked very hard with her physical therapy and has made a dramatic recovery,” Dr. Fahner said. “She has a wonderful family support system who has been behind her every step of the way. We all feel very blessed to care for Naomi and to get to know her family. It was looking quite tragic for a while and it turned into a success story.”



























 /a>
/a>
 /a>
/a>
 /a>
/a>
I know Naomi and her mom. I worked with her grandma and followed Naomi’s progress from thinking she wasn’t going to survive to now being back to school! What a miracle!
I followed Naomi praying that she be healed. My heart is a flutter with her story. I have one brave little cousin. I am hoping things continue to go well. 💕She is one brave child!!💕