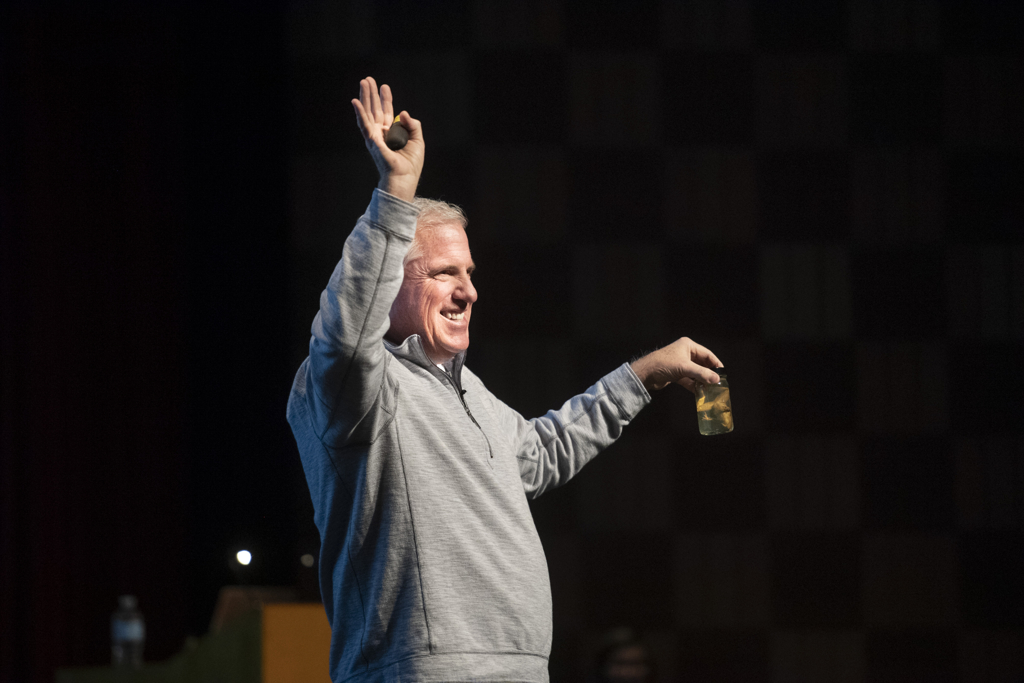
David Stults stood in front of a packed auditorium at Lowell High School recently, sharing his medical journey with students.
Even though the cause of his irreversible lung damage is, of all things, microwave popcorn, Stults has learned that vaping can cause similar damage. And he wants students to know it. Before they suffer a similar fate.
Stults, now 59, started feeling short of breath about 10 years ago when he’d go up and down the stairs at his house.
“Your initial thought is, OK, it’s time to push away from snacks and do some exercise, which I began to do,” the Walker, Michigan, resident said. “The symptoms only became worse. I went to my PCP. He listened to my lungs and said, ‘Something doesn’t sound right.’”
The doctor referred him to Michael Harrison, MD, a Spectrum Health pulmonology disease specialist.
In late 2009, lung function tests put Stults in the 70% to 80% range.
“For a healthy 49-year-old man, that was alarming,” Stults said. “Imaging showed some very ugly air trapping. He did all the breathing testing and put me on a pretty aggressive regimen of prednisone and inhalers.”
But time would not be a healer.
By February 2010, his lung function had worsened, dipping to the 60% range.
“It’s heading south quickly,” he said. “I was taking 60 to 80 milligrams of prednisone a day, as well as other inhalers. I started doing breathing treatments a couple of times a day.
“By March or April, I was down to 30%,” he said. “I couldn’t walk up half a flight of stairs without stopping to catch my breath. Any kind of incline was a challenge. Even the gentle incline of the drive walking from the mailbox to my home, I’d have to catch my breath.”
By May, he continued to slide downhill, requiring weekly pulmonology appointments.
Medical mystery
Dr. Harrison suspected Stults may be suffering from an autoimmune issue. A rheumatologist started aggressive treatment with Rituxan, a drug normally used to fight cancer.
“I felt great afterwards,” he said. “I had more energy. I didn’t feel as short of breath.”
The diagnosis came in May 2010: bronchiolitis obiliterans, a severe lung inflammation that is both progressive and irreversible.
Doctors confirmed the diagnosis after three days of intense testing.
He returned home on oxygen.
“They said, ‘You need to go home and get your affairs in order,’” Stults said. “My wife (Barb) and I are both very committed and devoted Christians. We reached out to our family and friends and let them know we were asking for prayer. I can tell you from that day forward, my lung capacity has increased from 41% to 43% and has never gotten worse.”
Still, Stults wondered how he could have contracted this untreatable condition.
Dr. Harrison asked if he had been exposed to insulation, factory or foundry chemicals.
No. Stults had always worked white collar jobs.
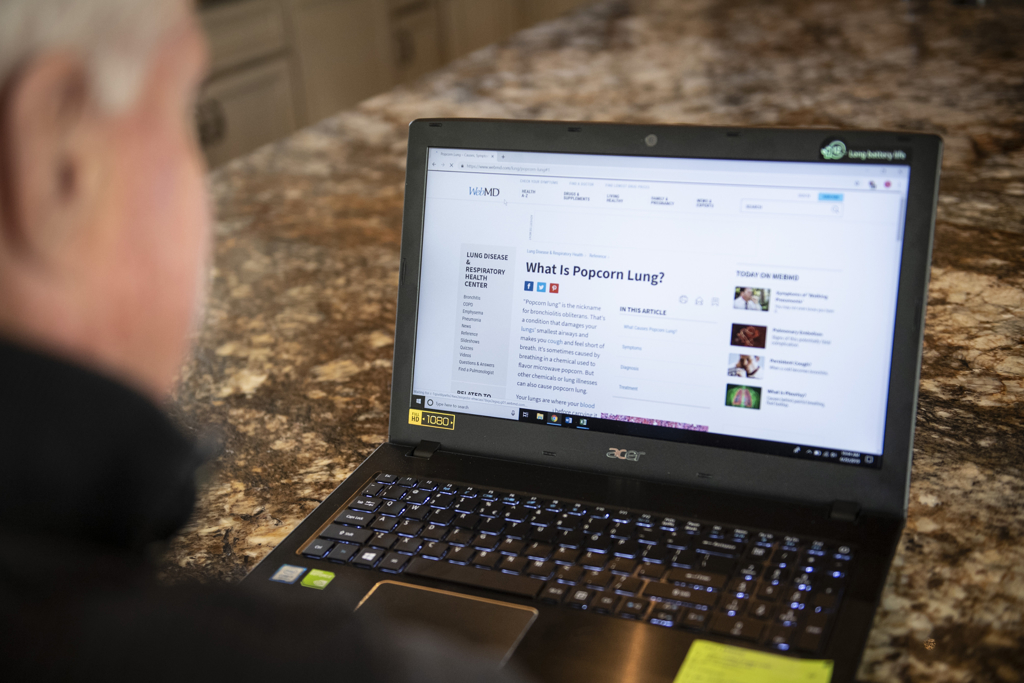
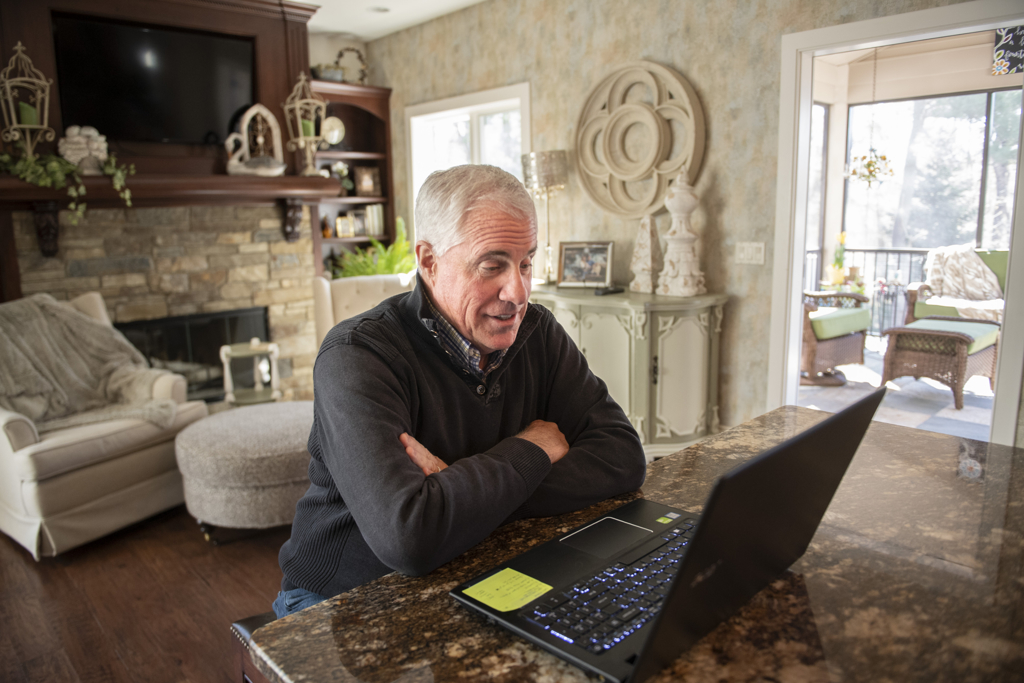
He launched a massive internet search on his condition.
“Up popped this article on popcorn lung,” Stults said. “It told the story of these plant workers at various microwave butter-flavored popcorn manufacturers who were dying at this incredibly crazy rate. It was only the employees in these cities, working at these plants. A dozen employees died over six months. It was ridiculous.”
Federal agencies such as OSHA and NIOSH launched an investigation and learned the chemical used to create the butter flavoring, diacetyl, when it’s heated, creates a potentially toxic vapor.
“My wife and I loved microwave butter-flavored popcorn,” he said. “My secretary at the office would make me a bag every day. I really enjoyed it, almost to an addictive level—opening the bag and sniffing in the fumes. I was breathing in the diacetyl on a daily basis. We had done that for 30 years.”
Stults’ condition may be irreversible and incurable, but he’s trying his best to reverse the actions of students who vape.
“We were talking with some friends of ours who are 20 years younger than we are and they have high school age boys,” Stults said. “She’s kind of the cool mom of Hudsonville. They have a nice home with an indoor basketball court. All of the guys in her son’s class hang out there.
“Because she’s so cool and engaging, the boys started to confess to her that a lot of them were vaping and couldn’t stop,” he said. “They were reaching out to an adult that they trust.”
She did some research and found that diacetyl is one of the many chemicals used to create different flavors in vaping pods.
“She knew my story and called me,” Stults said. “Besides nicotine, which is incredibly addictive, there’s asbestos and formaldehyde. You wouldn’t live with it in the attic and you’re going to suck it into your lungs?”
Snuffing out vaping
According to a series of national surveys recently released by the federal government, about 40% of high school seniors have vaped, double from the year prior.
Stults teamed up with Spectrum Health Medical Group pulmonologist Shelley Schmidt, MD, to set up talks at schools, with the goal of shining a light on the dangers of vaping pod chemicals and nicotine addiction.
“I get at least a phone call a week from a principal saying, We don’t know what to do. It’s out of control,’” Stults said. “Students are addicted. They don’t know how to stop.”
Stults aims to portray the real-life picture of what the chemicals do.
“I tell them, ‘Here’s what you’re setting yourself up for—40% lung capacity,’” he said. “Dr. Schmidt explains addiction and what’s going on in your lungs.”
Stults said they’ve only done a handful of presentations so far, but as principals talk to each other, engagement requests are growing.
“These kids do it walking down the hall in the school,” Stults said. “They do it in the classroom. They sneak it. Other than kind of a fruity smell, there are no fumes.”
Glenn VanOtteren, MD, a Spectrum Health Medical Group pulmonary disease specialist, said popcorn lung is rare but it could become more of an issue as vaping data becomes available.
“With the removal of diacetyl from heated food, we saw it rarely,” Dr. VanOtteren said. “We don’t have data on the rates of vaping-induced lung disease because the use of vaping has accelerated in the last two to three years.”
Dr. VanOtteren said Stults is doing well, despite limitations.
“His lung disease is stable,” Dr. VanOtteren said. “He is short of breath with stairs. He requires daily medicine and has flares of his disease about two times a year when he gets worse and needs additional medications. His lungs can continue to decline because of these flares.”
Dr. VanOtteren said he’s impressed Stults and Dr. Schmidt are sharing lung lessons with students.
“This is such a contemporary and important topic,” he said. “Providing education at this early age is super impactful.”















 /a>
/a>
 /a>
/a>
 /a>
/a>
We would be interested in having you speak at Belding Area Schools
Vaping is an epidemic in our schools. Anyone with school aged children knows how common this is and how quickly the next generation of kids are becoming addicted to nicotine. For all the good work we have done in this country to reduce cigarette smoking, the challenge of stopping our children from becoming addicted to vaping (or helping them quit) has become a public health emergency. Schools, healthcare systems, parents and other social leaders need to organize their message and help limit this growing problem.
Thank you to David Stults for sharing his story and Dr. Shelley Schmidt for providing the medical perspective on nicotine addiction. This message is a great example of individual efforts that can have a great impact on our community.
remember when they started selling these they said IT WAS SAFE and look how dangerous they are now.
Years ago, a vape shop opened near me. After several months of brisk business, I noticed, walking by, a greasy film on the windows and I asked the owner if vaping was dangerous. She said, its safe. End of discussion. So, I pointed to the windows and said, but that film on the windows….doesn’t that end up coating your lungs? She ignored my question. Now we know why.
Excellent observation, Maureen. Thank you for sharing this anecdote. Best, Cheryl
I teach in Traverse City, MI and know that there is an increase of vaping in our community and schools. Your story is very inspirational. This even hits close to home as one of my married sons vapes and thinks it is ok. Nothing we can say or do helps him to realize the dangers this can do to him. I am so glad to read that people like you are out telling and teaching our children of the dangers. Thanks you so much
Bravo Zulu my friend. Your story is amazing, and to present the hazards to others that you gained from your experience is second to none. My Best Wishes to you as you go forward with your message. Your Eldean dock friend, Lou