Amanda Rostic left her prenatal ultrasound appointment with questions swirling in her head.
She crossed the parking lot with phone in hand, searching for information on congenital heart defects. Her routine 21-week scan had revealed her unborn child had hypoplastic left heart syndrome.
“It was super serious,” she said. “The entire left side of the heart doesn’t form properly. Sometimes it doesn’t form at all.”
Despite the fear she felt in those first moments, it didn’t take long for Rostic to move from fear to action.
“In hindsight, I am grateful. One-third of families (of babies with congenital heart defects) don’t find out until after they are born,” she said. “When you know, you can plan.”
And that’s how Rostic has approached her son Harvey’s heart condition: with education, planning and a heart prepared to find the best in any situation.
“I think there’s always a silver lining if you look for it,” she said, as she sat in her living room, cuddling her infant son. “You’ve got to keep things in perspective.”
Harvey Parrott—nicknamed Handsome Harvey and Hero Harvey—wiggled, cooed and smiled up at his mother, brown eyes sparkling.
A casual observer might not realize this active, cheerful boy had a heart defect—except for the feeding tube in his nose. That’s often the case for kids with heart conditions, Rostic said.
And it’s one reason she didn’t realize how common congenital heart disease was before it affected her child. Now she’s eager to raise awareness and advocate for kids like Harvey.
“Every 15 minutes, a baby is born with a congenital heart defect. That’s 40,000 a year in the U.S.,” she said. “There are all sorts of rainbow hearts out there. I try to avoid the word defective. They are just different.”
A mind full of questions
Rostic, a pediatric research assistant for Spectrum Health, looked forward excitedly to the birth of her third child.
A veteran mom with energy to spare, she had an 11-year-old son, Cameron, and 3-year-old daughter, Helen. She knew well the ups and downs of child rearing—and childbirth. Helen arrived so quickly, Rostic delivered her in a car on the way to the hospital.
Learning about Harvey’s medical issues launched her onto a new parenting path.
After the ultrasound, she consulted with a team of Spectrum Health specialists in congenital heart disease, maternal fetal medicine and neonatalogy.
She made an appointment with Heather Sowinski, DO, a fetal cardiologist who works in the Helen DeVos Children’s Hospital Congenital Heart Center. Before they met, she emailed her a long list of questions. That was just fine with Dr. Sowinski.
“I welcome questions,” she said. “I think parents often feel they are overwhelming the physician with questions, but I think it’s great. It lets me know they understand what’s going on.”
Hypoplastic left heart syndrome is a rare condition.
“About 1 in 100 babies is born with a heart defect,” Dr. Sowinski said. “About 1 percent of them have hypoplastic left heart.”
Rostic underwent genetic testing before birth. Like 85 percent of children born with hypoplastic left heart, the test turned up no genetic syndrome or mutations that would account for the condition.
She met with Marcus Haw, MD, a pediatric heart surgeon, about the treatments available for her son. Typically, a child with hypoplastic left heart goes through a series of three surgeries to help the body compensate for the underdeveloped portion of the heart.
But individual circumstances can affect the treatment course, Dr. Haw explained.
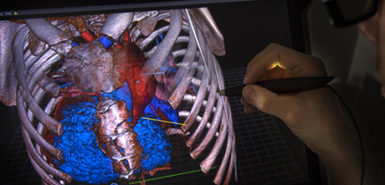
“I liked that he had a plan A, a plan B and a plan C,” Rostic said. “He drew everything out and explained everything to me.”
As it turned out, Harvey did not follow a standard course.
“Harvey does have hypoplastic left heart,” his mom said. “But he is definitely not your typical case.”
As expected, his left ventricle was small. That’s the chamber that is designed to pump blood to the body. Scans also showed the mitral valve, which controls blood flow on the left side of the heart, did not develop.
Harvey also had a condition called double-outlet right ventricle. Both of the big blood vessels that exit the heart were connected to the right ventricle. Typically, one connects with the left. He also had a hole in the wall between the upper chamber of the heart and a hole between the two lower chambers.
Despite his incredibly medically complex journey, Harvey is one of the happiest, most smiley babies you will ever meet.
After a smooth pregnancy, labor was induced and Rostic delivered Harvey at full term. On the small side, at 5 pounds, 7 ounces, Harvey also had a full head of curly dark hair.
“The (Neonatal Intensive Care Unit) team checked him out and he was fine, so we got to hang out a little bit,” she said.
Harvey was too small for the first surgery, which usually is performed when a baby is 1 week old. The operation, called a Norwood procedure, converts the right ventricle into the pumping chamber for the body.
Instead, the doctors gave him time to grow. They performed another procedure to improve his blood flow.
Dr. Haw teamed with Joseph Vettukattil, MD, a pediatric interventional cardiologist, to place a stent in Harvey’s heart. The two are co-directors of the Congenital Heart Center.
The stent kept open a connection between arteries that typically closes after birth. They also placed bands on the lung arteries to reduce the pressure on his lungs.
Three months later, Harvey was big and healthy enough for his Norwood procedure.
As he recovered from the surgery and some other complications, Rostic looked forward to the day she could bring her baby home for the first time.
That day came when Harvey turned 4 months and 29 days old. Rostic felt nervous. How would she handle the feeding tube? Replace it if it came out? Give her son injections?
“You can do it when you have to,” she said. “Now everything just seems like second nature.”
Back to tummy time
With each challenge, Harvey’s easygoing, happy nature made the transitions easier.
“His temperament is so chill,” Rostic said. “He is such a sweet baby.”
At home, Harvey continued to grow and put on weight. He charmed his big brother and sister. Even while juggling her son’s medical care and frequent checkups with his medical team, Rostic enjoyed peaceful days of family time.
“You always have to celebrate the little things,” she said. “Despite his incredibly medically complex journey, Harvey is one of the happiest, most smiley babies you will ever meet.”
At 7 1/2 months, Harvey was ready for the second big operation to reconstruct his heart. Called the Glenn procedure, it involves rerouting the blood that flows from the upper part of the body to the heart.
“From a heart standpoint, he has much more stable physiology now,” Dr. Sowinski said. “His oxygen level is higher and that helps with exercise tolerance and development.”
In his room in the pediatric cardiac intensive care unit at Helen DeVos Children’s Hospital, Harvey lay sleeping as his mom watched over him. She talked about all the caregivers involved in his bringing him this far—cardiology, neurology, hematology, nursing and physical therapy.
“When you look at all the steps, it really is some fascinating stuff,” she said.
For Harvey, the next big step is expected around age 4. His doctors plan to perform a Fontan procedure.
While balancing work, child care and Harvey’s medical challenges, Rostic has continued her efforts to advocate for children with congenital heart disease.
In February, based on a petition she submitted, Michigan Gov. Gretchen Whitmer issued a proclamation declaring Feb. 7-14, 2019, Congenital Heart Defect Awareness Week.
For Harvey, recovered from his latest operation, life is full of toys and fun.
“We can do tummy time again,” Rostic said. “He tries to blow raspberries. He’s good at reaching for things. He likes all things that are bright and noisy.
“Life has resumed as normal. He is as smiley and playful as ever.”















































 /a>
/a>
 /a>
/a>
 /a>
/a>
Love Handsome Harvey! He is one of the easiest going babies I have ever taken care of! Great job Amanda!
We love handsome Harvey! He is such a sweetheart! Just the cutest little guy you ever did see! Congratulations Rostic family!!
So true, Brianna and Kristen! We were so charmed by Harvey, with his bright eyes and happy smile.