The initial panic of COVID-19 may be lightening, but the heavy lifting continues for those working the front lines of a global pandemic.
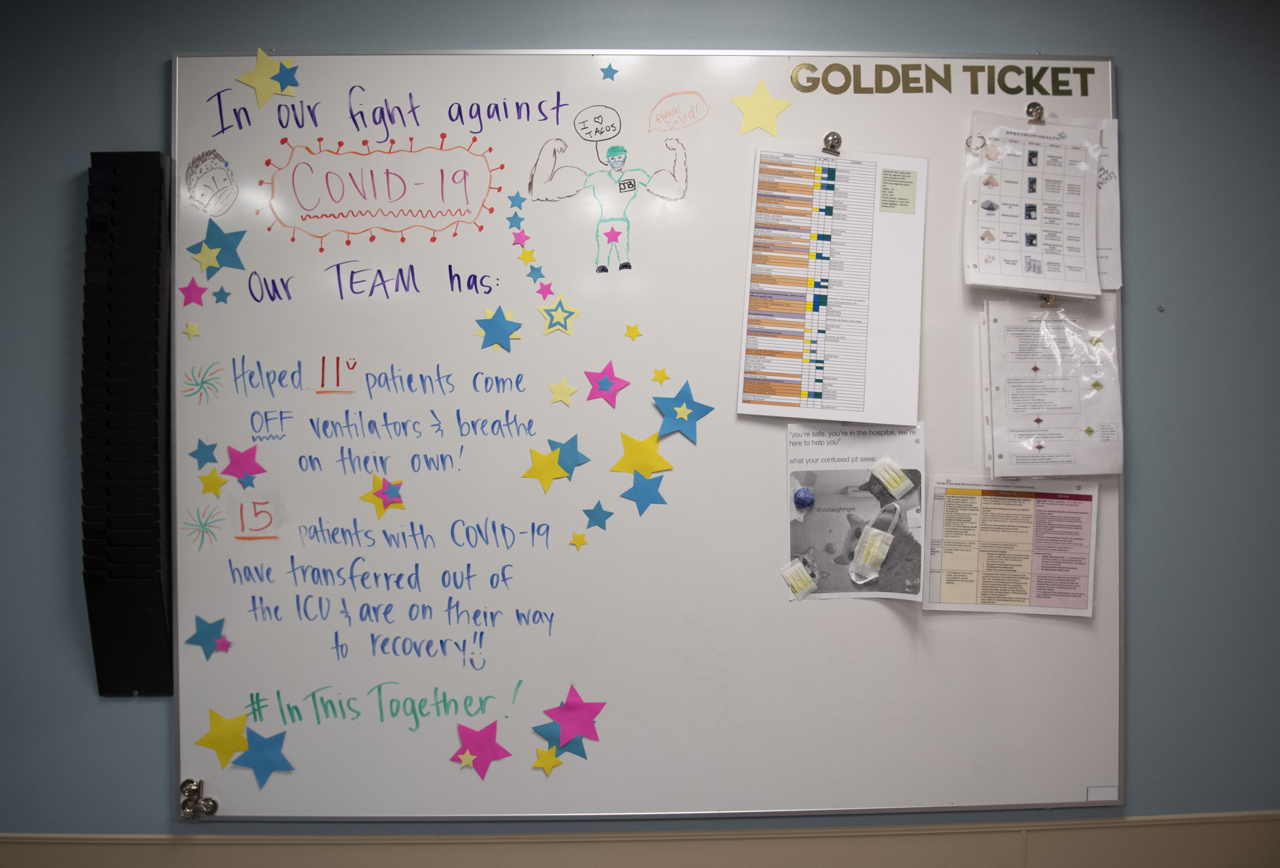
Spectrum Health Blodgett Hospital intensive care unit team members—from physicians, pharmacists and phlebotomists to nurses, nutritional and environmental services experts—continue to work together in an attempt to fight back against the virus.
They’ve been close to COVID-19. They’ve witnessed the suffering, the complications, but they’ve also delighted in what they call the “code happy” of patients who have recovered. Through it all, they symbolically locked arms in solidarity, ICU comrades versus COVID-19.
ICU nurse manager Audra Nelson-Arnett, MSN, RN, said she’s proud of the ICU team.
“The staff were called upon during a most stressful time, to provide care and compassion to COVID patients, as well as support their own teammates,” Nelson-Arnett said. “The hospital staff were the only people these COVID patients would see, sometimes for weeks. I believe the staff, no matter their own personal fears or trepidations, stepped into those COVID rooms with confidence, positivity and bravery, to ensure the best outcome for the patient.”
It hasn’t been easy. Far, far from it.
“Nursing is not an easy job, but when you see someone recover and leave the ICU, it is the best reward,” Nelson-Arnett said. “They are a close-knit team and support each other well. Their desire to help people also keeps them going.”
In the past six months, these Blodgett Hospital ICU team members may have grown more comfortable with their daily tasks, but they all shared a common message—take this disease seriously.
These are their stories.
Elyse Green, RN
“For a short period of time, COVID patients were all that we had for the most part,” Green said. “We didn’t have a lot of patients on the unit because people were not coming into the hospital and hospitals weren’t doing surgeries.”
That’s all changed since surgeries and other procedures are back on the docket.
The early days were the scariest days. Health care workers, and the general population, simply didn’t know much about the virus. They’re learning, still.
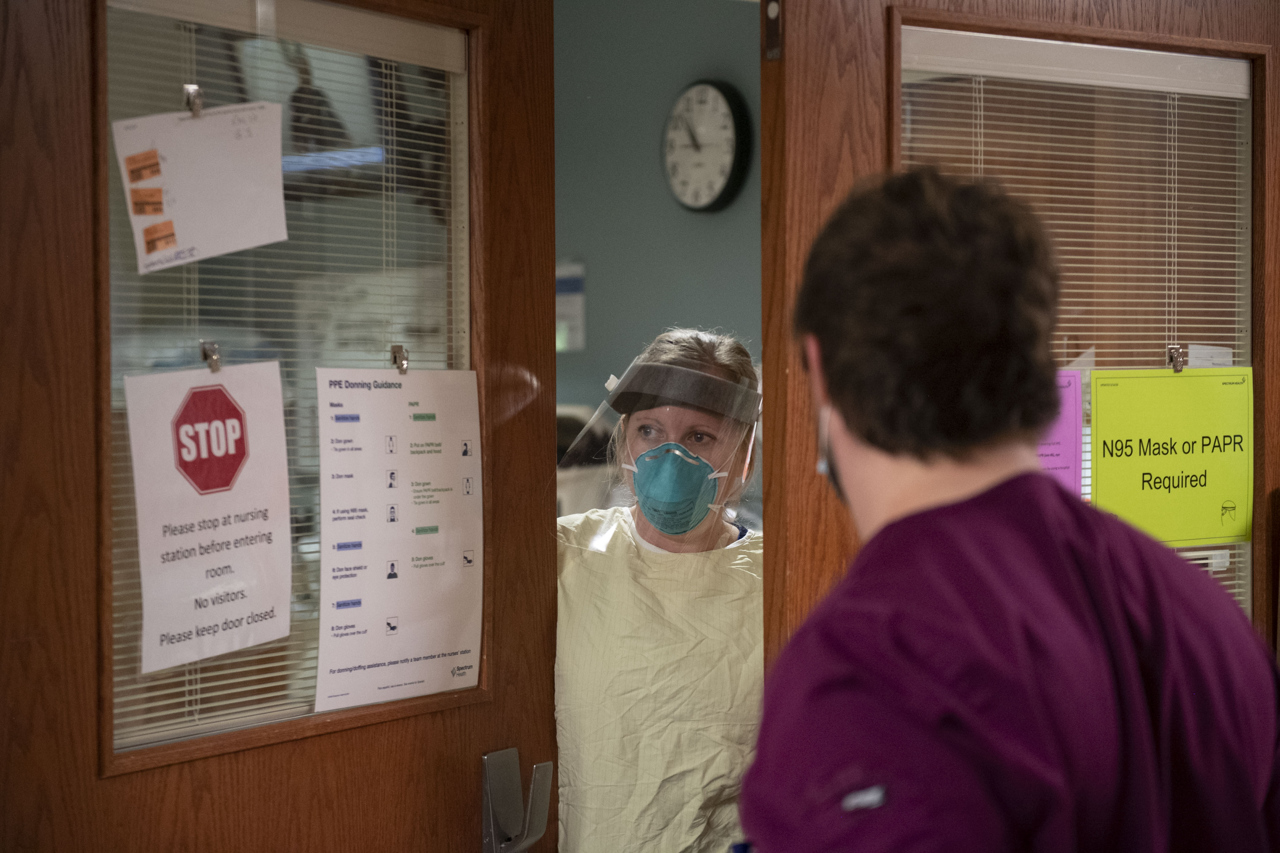
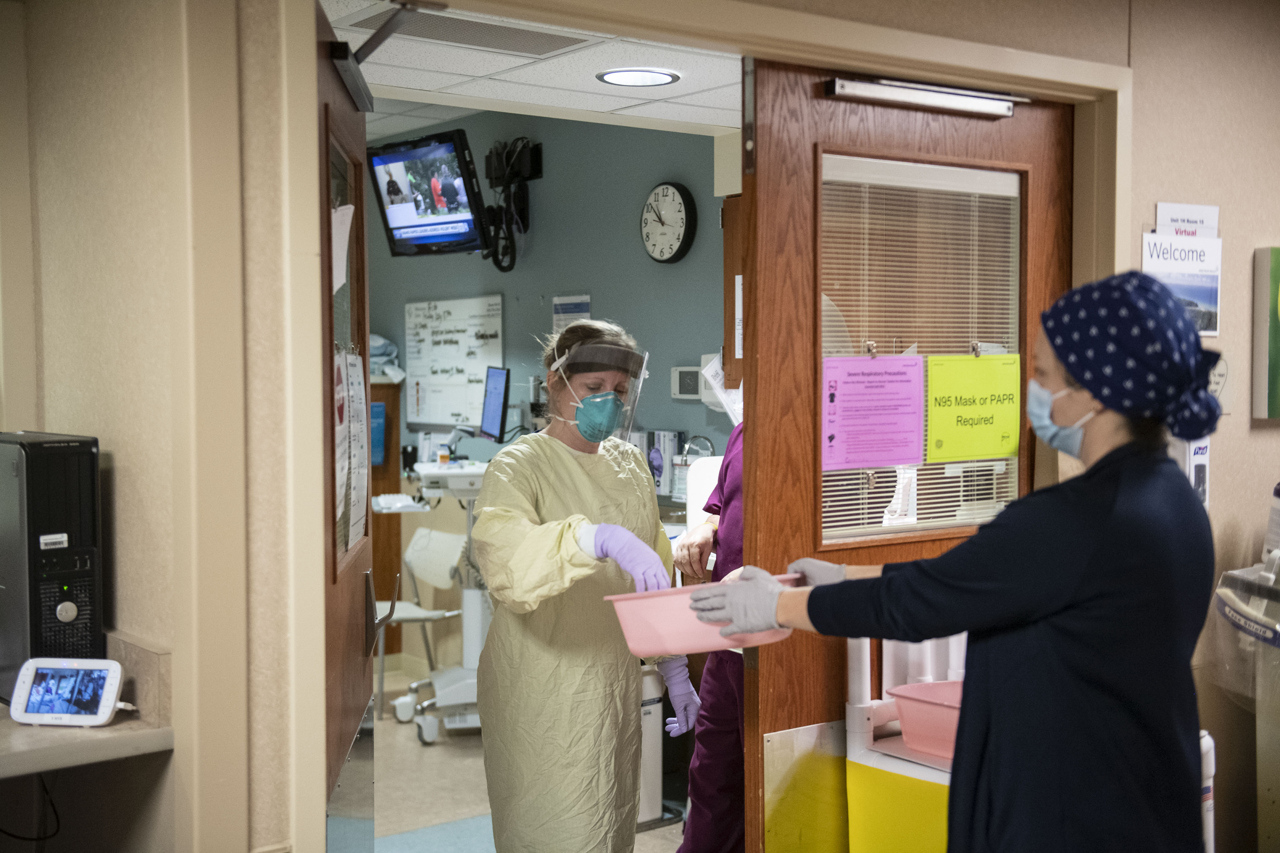
When caring for people who have COVID-19, team members wear N-95 masks, face shields, gowns and gloves. There’s a strategic order for putting them on and taking them off.
The disease isn’t the only thing patients battle. Many fight loneliness. Hospital patients who test positive for COVID-19, due to exposure risks, aren’t allowed to have visitors. They instead communicate with family members through an iPad.
We are the only people these patients see in person in a day, Green said. “We’re the ones going in and out.”
Vicky Lowing, laboratory services phlebotomist
In 27 years working in health care, Lowing said she’d never been scared. Until COVID-19. The virus changed her perspective and deepened her awareness of her surroundings.
“Every move you make in a COVID room you doublethink it,” Lowing said. “In 27 years, I’ve never worried and I’ve been through a lot of different viruses.”
The precautions are many.
“We have one assigned COVID phlebotomist, but it’s so time-consuming the rest of us have to pick up the slack at times,” she said.
She typically draws blood in the morning. She celebrates the happy COVID-19 case conclusions. But that’s not always the case.
“Sometimes it’s sad,” Lowing said. “It doesn’t always go the way you hope it would, but there are a lot of happy times, too. Patients do leave. They get off the respirator and they make it. We work very hard to get them that way and we don’t take it lightly.”
She used to.
“In the beginning, I took it very lightly,” Lowing said. “I thought, ‘This is just another virus and it’s going to go away.’ The more I got into it, I got scared. I was afraid. Wear the mask. Do the social distancing, protect yourself and don’t take it lightly. It’s here.”
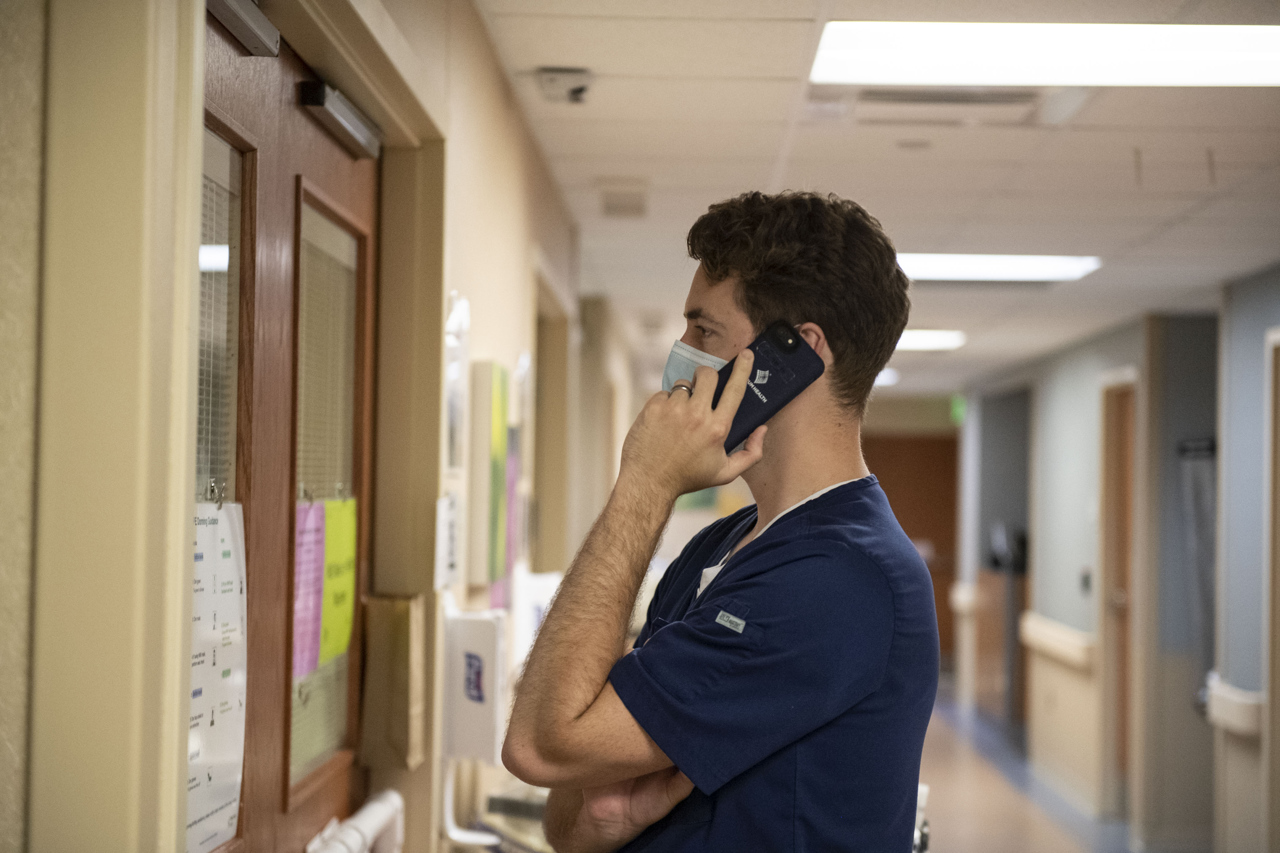
Eric Cooper, RN
For Cooper, who started as an ICU charge nurse a year ago, the biggest change has been the reality of living in a worldwide pandemic. And getting used to working through it.
“We come from a baseline level of fear that we all started with to getting more comfortable,” Cooper said. “At this point, we’re pretty straightforward and comfortable with it. It’s better than always being afraid.”
Cooper said as team members adjusted and got used to PPE and procedures, they discovered their new normal.
“It just flows a lot better now,” he said. “COVID, we discovered, is very long-lived. A lot of (patients) are intubated and sedated for a long time. When they start getting better and interact, we get to know who they are and what they value.”
One patient spent a month and a half in their ICU.
“A lot of staff didn’t expect him to make it through,” Cooper said.
As the patient slowly recovered and started to communicate, Cooper and other team members helped him reach out to family on an iPad for virtual visits.
“It was special to see what we could do to help him get better through that huge course,” Cooper said. “A lot of people said, ‘He’s not going to make it,’ but he more or less recovered right in front of us. By the time he was leaving our unit, he could talk and he was eating food. He was probably one of our sickest patients. We had multiple conversations with the family saying, ‘This is probably not going to end well.’ He swabbed negative finally and he’s in the rehab unit.”
The man’s recovery provided a huge boost for team members.
Not everyone is so lucky. Cooper said after seeing what they see on a daily basis, he grows frustrated when people don’t take COVID-19 seriously.
“It’s super frustrating going out in public and seeing people who don’t believe and don’t seem to care to wear a mask,” he said. “This stuff is real. People are dying from this. The biggest thing is, we’re still in this. Things have gotten better, at least in this area, but it’s still a risk. People forget that as they get complacent and get restless in what the world’s become.”
Complacency could equate to more power for COVID-19, to a greater viral spread.
“If we don’t take this seriously, we’re going to be back where we were,” Cooper said. “We have more supplies these days, but we don’t want to test those supplies.”
Tiffany Yenior, environmental services
Yenior cleans ICU rooms, including those that house patients battling COVID-19. She dons a gown, mask, face shield and gloves before entering.
“I worried at first because I have a young child at home,” Yenior said. “It was very nerve-wracking. I didn’t even know what I was getting myself into.”
During the past six months, she’s grown used to the routine and appreciates the team support.
“They welcomed me like family,” she said. “They’ve all been super supportive and they’ve had my back making sure we’re all doing good and staying safe.”
If patients are able to talk, Yenior said she carries on conversations while she’s cleaning, fully aware the patients are not able to have families in the rooms as they battle the virus.
“I think it really makes their day having a conversation,” she said.
Yenior said her best days are when she sees a patient recover and leave intensive care.
“You can’t see it under the mask, but I smile when I hear that,” she said. “You never know what’s going to happen. It’s good they get to go home and see their families again. It fills my heart with joy for them.”
She also wishes they’d never landed in the ICU in the first place.
“I don’t want to see anybody in here,” Yenior said. “(COVID’s) definitely a serious deal whether anybody believes it or not. I see it every day. It would definitely help slow this down and get rid of it if we’re all wearing masks, washing hands and practicing our distancing. Definitely take this seriously for sure and keep that mask on.”
Brittany Stutzman, RN
Stutzman said she’s thankful to be surrounded by a supportive team of medical professionals in the ICU.
“We’ve definitely experienced some transitions in the last few months,” Stutzman said. “It’s nice we can all rely on each other when we’re going through the changes and unknowns. Early on in March and April there were some moments of being overwhelmed and intimidated because it was so new to us. It was definitely unnerving not knowing what kind of day you would walk into or what it would be like.”
The team worked together, one day at a time.
“It’s a little more familiar at this time,” she said. “We still rely on each other a lot to care for the really sick patients.”
Stutzman said team members also prepared for a surge in COVID-19 cases.
“It was scary to think about that happening here,” she said. “We weren’t sure when it was going to hit and we were almost bracing for the impact at times. Thankfully, we never experienced that fully here, but I think we felt prepared.”
Stutzman remembers one patient who stayed in her unit for several weeks.
“At times, we weren’t sure how it would end up,” she said. “Every day, little by little, the patient is making progress. They moved out of our facility not requiring any oxygen.”
Stutzman said she and her team adjust ventilator settings as patients begin to recover.
“We make changes to test them to see if they can do more work on their own and have less support from the ventilator,” she said.
Speaking of support, Stutzman said the outpouring of compassion and support from the community has inspired her and her team.
“The small messages and the way food was sent in was a big morale booster during the scary unknown times early on,” she said.
Stutzman reminds everyone to remain vigilant in fighting the virus.
“Wearing a mask is such a simple act of support,” she said. “Please wear a mask. It is such a small way to help.”
Katie Milanowski, clinical pharmacist
Milanowski said COVID-19 is a moving target.
“Drug therapy has changed throughout the course of COVID,” she said. “We’re working with physicians, the pharmacy department, infectious disease specialists, we all work together. Whatever the current research is showing is what we use in our practice. We’ve been monitoring the leading edge of studies.”
Milanowski said they stock a small supply of a COVID-19 investigational drug for patients who are eligible and meet select criteria.
She delights in seeing patients recover from the virus, a term she calls “code happy.”
Recovered patients either go home or to a rehabilitation unit.
“They can pick celebratory songs and we play them overhead so everyone can share that moment with them,” Milanowski said. “It is uplifting. It’s nice to hear that someone has recovered and is moving forward.”
Throughout the pandemic, team members have learned much—from and about the virus.
“It’s something new, something we haven’t seen before,” she said. “I see the doctors becoming students of the virus. They learn how it works, learn the course and figure out how to combat the virus and support the patient through the virus.”
Milanowski said the ICU has treated all ages of adults with COVID-19.
“The virus is working its way around, and some of us or our loved ones are at risk for complications,” she said. “Take care of yourself with plenty of sleep, healthy food, exercises and staying in touch with family and friends virtually. The best way to get through a time like this is to unify, and share the load with friends and co-workers. We are all in this together.”




















 /a>
/a>
 /a>
/a>
 /a>
/a>
Proud of my son and all those working on the COVID front lines!
Thank you front line teammates for continuing to give your best every day!!
This is a cool article. Thank you!
My husband and I were Covid 19 patients at the same time.and my husband of 53 years passed away while there and I went home recovering after almost 3 weeks as an inpatient. The staff in the Covid 19 area and in ICU were so compassionate during the most difficult time in our lives and I think of them every day and what they sacrifice for us. I will never be able to thank them enough.
Pamela, I’m truly so very sorry for your loss. Thank you for your kind comments and support for our team members. Your thoughtfulness means the world to them. Please know we’re thinking of you and wishing you wellness and peace.